When bile flow stalls, patients face itching, fatigue, and a ticking clock toward liver failure. Ursodeoxycholic Acid offers a way to reset that clock, especially for people battling cholestatic liver diseases. This guide explains what the drug does, why it matters, and how doctors use it to keep livers functioning longer.
What Is Ursodeoxycholic Acid?
Ursodeoxycholic Acid is a hydrophilic bile acid originally isolated from the bile of bears. It is now synthesized and sold under brand names like Ursodiol and Actigall. Its primary role is to modify the bile‑acid pool, making it less toxic and promoting smoother bile flow.
Unlike the more aggressive bile acids the liver normally produces, UDCA is gentle on cell membranes and can protect cholangiocytes-the cells lining the bile ducts-from damage.
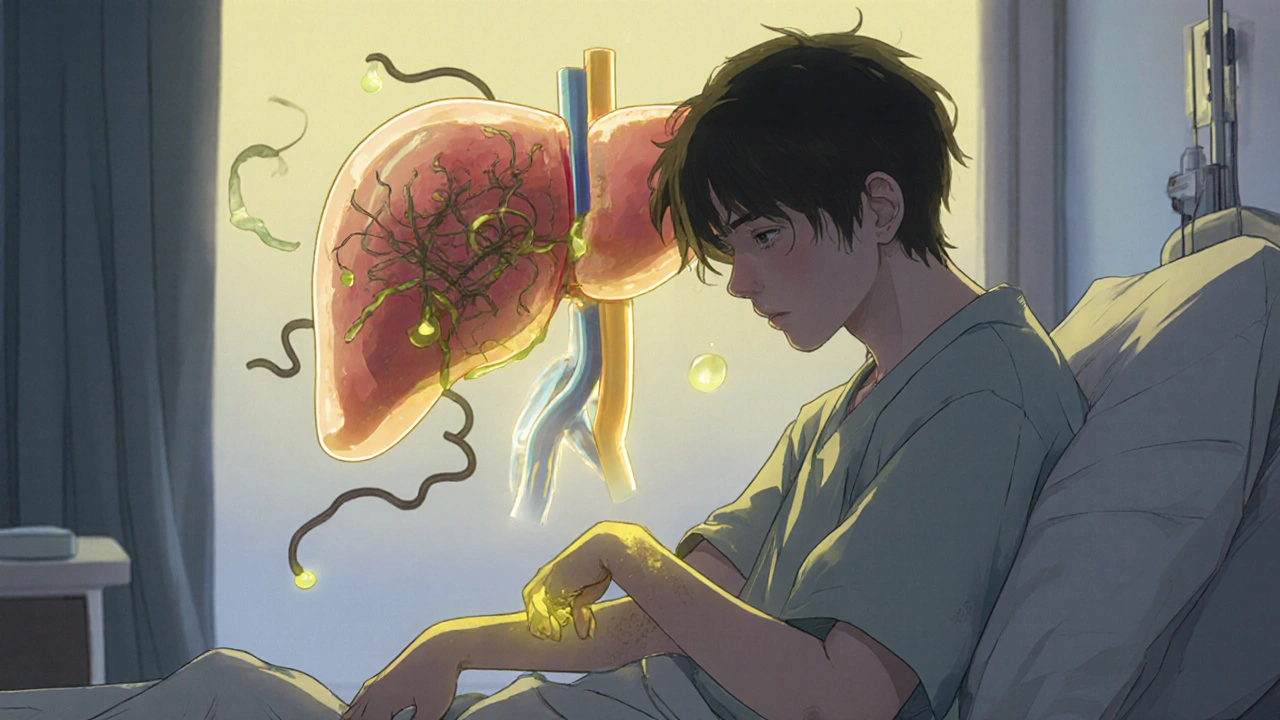
Understanding Cholestatic Liver Diseases
Cholestatic Liver Diseases are a group of disorders where bile cannot move properly from the liver to the intestines. The most common forms are Primary Biliary Cholangitis (PBC) and Primary Sclerosing Cholangitis (PSC). Over time, cholestasis triggers inflammation, fibrosis, and ultimately cirrhosis.
Patients often present with jaundice, pruritus, and elevated liver enzymes-especially alkaline phosphatase.
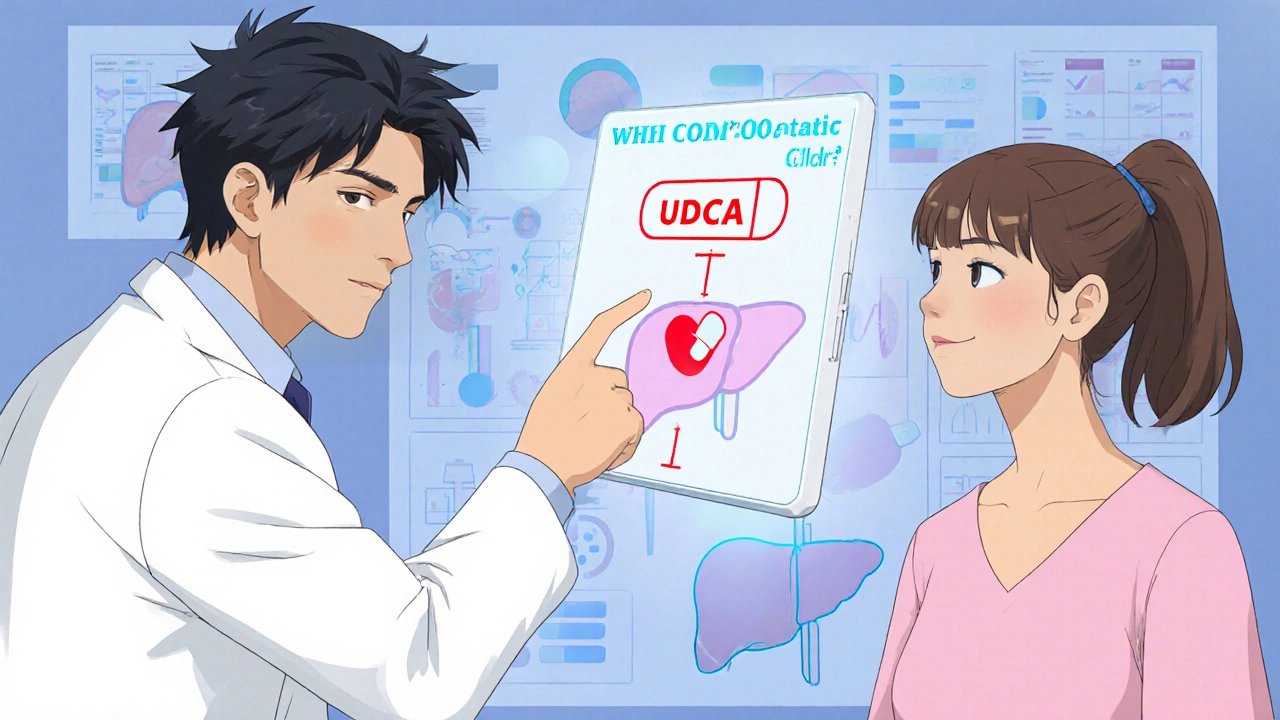
How UDCA Works in the Liver
The drug tackles cholestasis on three fronts:
- Choleresis: It stimulates the secretion of bile, helping to flush out toxic acids.
- Cytoprotection: By replacing harmful hydrophobic bile acids, UDCA reduces oxidative stress on liver cells.
- Immunomodulation: It dampens the immune attack on bile‑duct cells, a key driver in PBC.
These mechanisms translate into measurable drops in serum alkaline phosphatase and bilirubin, two markers doctors watch closely.
Clinical Evidence: What the Trials Show
Large, multicenter studies have cemented UDCA as first‑line therapy for PBC. In the 1994 Mayo Clinic trial, 1,000 mg daily for two years reduced the risk of liver transplantation by 30 % compared with placebo.
For PSC, the picture is more nuanced. A 2017 European cohort showed modest biochemical improvement but no clear survival benefit, leading most experts to reserve UDCA for patients with early disease or significant pruritus.
Key endpoints across trials include:
- Normalization of alkaline phosphatase (< 1.5 × ULN)
- Stabilization of MELD score
- Delay or avoidance of liver transplant
Dosage, Safety, and Monitoring
Typical adult dosing ranges from 13‑15 mg/kg/day, divided into two doses. Pediatric regimens hover around 20 mg/kg/day.
Side‑effects are generally mild-diarrhea, nausea, or headache. Rarely, patients develop hepatotoxicity, so routine lab checks are essential.
Monitoring schedule:
- Baseline liver panel, including alkaline phosphatase, ALT, AST, bilirubin.
- Repeat labs at 3‑month intervals for the first year.
- After 12 months, if alkaline phosphatase stays < 1.5 × ULN, extend interval to every 6 months.
Patients who fail to achieve biochemical response after one year may need additional therapy, such as Obeticholic Acid.
Comparing UDCA with Other Options
| Attribute | Ursodeoxycholic Acid | Obeticholic Acid | Placebo |
|---|---|---|---|
| Mechanism | Hydrophilic bile‑acid replacement, choleresis | FXR agonist, reduces bile‑acid synthesis | None |
| Typical Dose | 13‑15 mg/kg/day | 5‑10 mg once daily | - |
| Alkaline Phosphatase Reduction | 30‑45 % | 15‑25 % | 0 % |
| Pruritus Relief | Moderate | Variable (can worsen itching) | None |
| Transplant‑Free Survival (5 yr) | ~70 % | ~65 % | ~55 % |
Both drugs are approved for PBC, but the safety profile of UDCA makes it the go‑to first line. Obeticholic Acid is added when UDCA alone doesn’t achieve biochemical targets.
Practical Prescribing Guide
When considering UDCA, clinicians follow a simple decision tree:
- Confirm diagnosis of cholestatic disease (PBC/PSC) via imaging, antibodies, and liver biopsy if needed.
- Check baseline labs-especially alkaline phosphatase and MELD score.
- Start UDCA at 13‑15 mg/kg/day. Adjust for renal impairment or weight extremes.
- Re‑evaluate labs at 3 months. If alkaline phosphatase < 1.5 × ULN, continue.
- If no response, discuss adding Obeticholic Acid or enrolling in clinical trials.
- Educate patients about potential side‑effects and the importance of adherence.
Key checkpoints for follow‑up:
- Adherence rate > 80 %
- Stable or improving MELD score
- Absence of new jaundice or ascites
When disease progresses despite optimal therapy, referral for transplant evaluation becomes inevitable. Liver Transplant offers a definitive cure but carries its own risks and lifelong immunosuppression.
Common Questions About UDCA
Can I take UDCA if I’m pregnant?
Pregnancy studies are limited, but most hepatologists consider UDCA safe in the second and third trimesters when the benefits outweigh unknown risks. Always discuss with your obstetrician‑hepatology team.
What if I experience itching that worsens on UDCA?
Mild pruritus is common. Antihistamines, cholestyramine, or dose adjustment can help. If itching becomes severe, your doctor may add a low‑dose FXR agonist or switch to Obeticholic Acid.
How long do I need to stay on UDCA?
For chronic cholestatic diseases, UDCA is typically a lifelong therapy unless a liver transplant occurs or the disease resolves, which is rare.
Is UDCA available over the counter?
No. It’s a prescription‑only medication in most countries because dosing needs careful adjustment and monitoring.
Can UDCA interact with other drugs?
Yes. It can increase serum levels of cyclosporine and some anticoagulants. Always share your full medication list with the prescribing physician.
Bottom Line
For patients with cholestatic liver diseases, especially Primary Biliary Cholangitis, Ursodeoxycholic Acid stands as a proven, well‑tolerated option that slows disease progression, relieves itching, and reduces the need for transplant. When used correctly-right dose, regular labs, and timely escalation-it can be the difference between a stable life and a rapid decline.
Deanna Williamson
October 26, 2025 AT 18:33The pharmacokinetic profile of UDCA demands vigilant dose adjustment, especially in patients with variable body mass indices; otherwise, sub‑therapeutic exposure may masquerade as treatment failure. Moreover, the article glosses over the fact that alkaline phosphatase normalization alone does not guarantee histologic improvement. A more nuanced discussion of endpoint selection would have been appropriate.
Carolyn Cameron
October 27, 2025 AT 01:30In an effort to elucidate the mechanistic distinctions, one must acknowledge that UDCA functions as a hydrophilic bile acid surrogate, thereby attenuating cholangiocyte apoptosis through membrane stabilisation. The comparative table, while informative, omits the pharmacodynamic nuances that differentiate FXR agonism from choleresis. A rigorous appraisal would benefit from a deeper exploration of these pathways.
Samantha Taylor
October 27, 2025 AT 08:26Ah, the perennial saga of UDCA – touted as the panacea for cholestasis, yet the literature is riddled with caveats that the casual reader often overlooks. Firstly, the Mayo Clinic trial you referenced, while pivotal, enrolled a highly selected cohort with early‑stage PBC, thereby limiting external validity. Secondly, the biochemical endpoints, such as alkaline phosphatase reduction, are surrogate markers that do not uniformly translate to long‑term survival benefits.
Thirdly, the dosage range of 13‑15 mg/kg/day, though standard, fails to account for inter‑patient variability in hepatic metabolism, particularly in those with concomitant renal insufficiency.
Fourth, the safety profile, though generally favorable, includes rare instances of hepatotoxicity that necessitate monthly liver panel monitoring beyond the first year.
Fifth, the notion that UDCA is universally ineffective in PSC is an overstatement; recent meta‑analyses suggest modest symptom relief in a subset of patients with early disease.
Sixth, the article neglects drug‑drug interaction nuances, especially with cyclosporine and certain anticoagulants, which can precipitate clinically significant adverse events.
Seventh, the absence of discussion on patient adherence – an often‑underestimated determinant of therapeutic success – is a glaring omission.
Eighth, the economic implications of lifelong therapy are non‑trivial and should be factored into treatment algorithms.
Ninth, emerging data on combination therapy with obeticholic acid hint at synergistic effects, a point worth mentioning.
Tenth, the role of UDCA in prenatal settings remains controversial, with only limited data supporting its safety in the second and third trimesters.
Eleventh, the article's table, while handy, lacks confidence intervals, rendering the comparisons statistically ambiguous.
Twelfth, the narrative fails to address the psychological burden of chronic pruritus, which can be as debilitating as the biochemical abnormalities.
Thirteenth, the potential for UDCA to modulate gut microbiota – an area of growing interest – is ignored.
Fourteenth, the impact of genetic polymorphisms on drug response is an emerging field that deserves attention.
Fifteenth, the simplistic dichotomy of “responders” versus “non‑responders” obscures the spectrum of partial responses that clinical practice routinely encounters.
Finally, while the article correctly emphasizes the importance of early intervention, it could have been enriched by a discussion of real‑world implementation challenges.
In sum, UDCA remains a cornerstone of cholestatic disease management, but its application is far more intricate than the brief overview suggests.
Joe Langner
October 27, 2025 AT 22:20Honestly, UDCA is like a good cup of coffee for the liver – it wakes things up without the bitter aftertaste. When you think about the liver as a philosopher, it's always seeking balance, and this drug nudges it toward harmony. Sure, you have to keep an eye on labs, but that’s just part of the journey, right? Keep the faith and stick with the regimen; the liver will thank you.
Ben Dover
October 28, 2025 AT 05:16While the optimism expressed above is commendable, one must not overlook the empirical evidence indicating that UDCA’s efficacy is contingent upon strict adherence to dosing protocols. Deviations, even minor, can precipitate suboptimal outcomes, thereby undermining the therapeutic intent. A rigorous, data‑driven approach remains indispensable.
Katherine Brown
October 28, 2025 AT 12:13In the spirit of constructive dialogue, I wish to acknowledge both the therapeutic merits of UDCA and the necessity for patient‑centered monitoring. Open communication between clinician and patient can mitigate misunderstandings regarding side‑effects and reinforce adherence.
Leah Ackerson
October 29, 2025 AT 02:06It's fascinating how some still view UDCA as a miracle drug 🙄. In reality, its benefits are modest and highly patient‑specific. Let's keep expectations realistic and focus on comprehensive care. 🌱
abidemi adekitan
October 29, 2025 AT 09:03Friends, think of UDCA as a gentle river that smoothes the stones in our hepatic landscape. By flowing steadily, it carries away the harsh acids, allowing the liver to breathe. Embrace the rhythm, check those labs, and let the river do its work.
Barna Buxbaum
October 30, 2025 AT 05:53Quick tip: when prescribing UDCA, split the daily dose into two administrations to improve tolerability. Also, remind patients to report any worsening itchiness promptly – a simple adjustment can make a big difference.
Alisha Cervone
October 30, 2025 AT 12:50Looks okay.
Diana Jones
October 30, 2025 AT 19:46Alright, let’s get technical: adherence rates above 80 % correlate with normalized alkaline phosphatase, which is the golden KPI for UDCA therapy. If you’re not hitting that target, consider dosage tweaks or adjunctive agents – the data doesn’t lie.
Abbey Travis
October 31, 2025 AT 04:06We’ve covered a lot of ground. Remember, the best outcomes arise from a partnership between patient education, regular monitoring, and personalized adjustments. Keep the conversation open and the liver happy.