Most people think type 2 diabetes is just about high blood sugar. But the real story starts long before the numbers climb. It begins with your body’s cells shutting the door on insulin - a hormone meant to help glucose enter and fuel your muscles, liver, and fat tissue. This is insulin resistance, and it’s the silent engine driving type 2 diabetes and metabolic syndrome. By the time a doctor says you have diabetes, your body has been fighting this battle for years - often a decade or more.
What Happens When Insulin Stops Working
Insulin isn’t just a key to unlock glucose into cells. It’s a signal. When you eat, your pancreas releases insulin to tell your body: time to store energy. But in insulin resistance, your liver, muscles, and fat cells stop listening. Glucose piles up in your blood. Your pancreas tries to compensate - pumping out more and more insulin. This is called hyperinsulinemia. For a while, it works. Blood sugar stays normal. But eventually, the beta cells in your pancreas get worn out. They can’t keep up. That’s when fasting glucose hits 126 mg/dL or higher - the official line into type 2 diabetes.
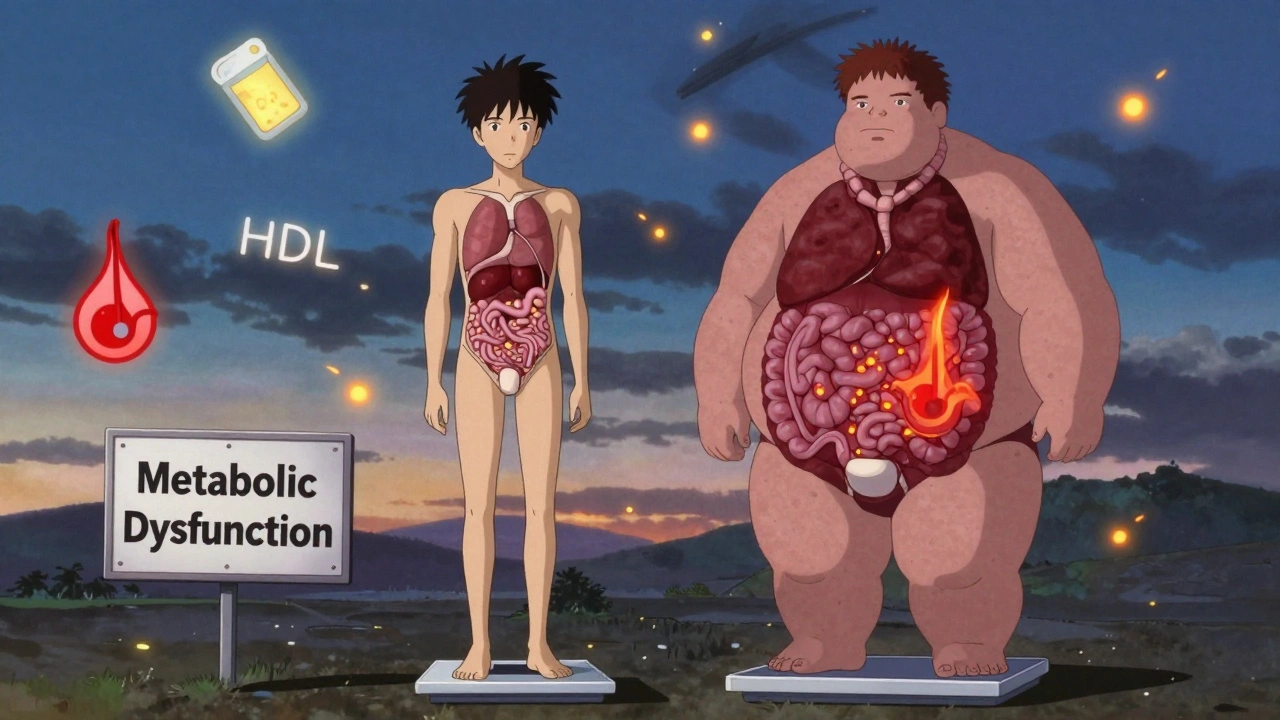
This isn’t just about sugar. High insulin levels trigger fat storage, especially around your belly. They raise blood pressure. They lower good cholesterol (HDL) and spike bad triglycerides. That’s the full picture of metabolic syndrome - not a single disease, but a cluster of warning signs your body is breaking down. The International Diabetes Federation says you have it if you have at least three of these five: waist size over 94 cm for men (or 80 cm for women), triglycerides above 150 mg/dL, HDL below 40 mg/dL (men) or 50 mg/dL (women), blood pressure at or above 130/85 mmHg, and fasting glucose over 100 mg/dL.
Why Metabolic Syndrome Is More Than Just Obesity
You don’t have to be overweight to have metabolic syndrome. And not everyone who’s overweight has it. The difference? Where the fat sits. Fat under the skin (subcutaneous) is mostly harmless. Fat inside your belly (visceral) and inside your liver is the problem. That’s the fat that releases inflammatory chemicals, blocks insulin signals, and floods your bloodstream with fatty acids. Studies show that 30-40% of obese people never develop metabolic syndrome - their fat is stored in the right places. Meanwhile, some lean people, especially those of South Asian descent, develop insulin resistance and diabetes despite a normal BMI. Genetics, diet, and activity levels shape where your body stores fat - and whether it turns toxic.
And here’s something most people don’t realize: metabolic syndrome isn’t just a pre-diabetes label. It’s a heart disease alarm. People with all five components have a 200-300% higher risk of heart attack or stroke than those with none. It’s not the sum of the parts - it’s the synergy. High insulin, high blood pressure, and abnormal fats together damage blood vessels in ways that none of them could alone.
The Shift from Syndrome to Dysfunction
Doctors are starting to drop the term “metabolic syndrome.” Why? Because calling it a “syndrome” makes it sound like a list of symptoms - something you just have. The new term, metabolic dysfunction syndrome (MDS), reflects what’s really happening: your metabolism is broken. It’s a disease state, not a collection of risk factors. The European Association for the Study of Diabetes plans to update guidelines in 2025 to reflect this shift. The change isn’t just semantics. It’s about urgency. If you have MDS, you don’t need to wait for diabetes to develop before acting. You’re already in danger.
One of the clearest signs of metabolic dysfunction is nonalcoholic fatty liver disease (NAFLD). Up to 70% of people with type 2 diabetes have it. If it progresses to NASH - where the liver gets inflamed and scarred - your risk of developing diabetes doubles. That’s why liver scans are now part of the routine check for anyone with insulin resistance.
How You Get There - And How You Can Turn It Around
There’s no mystery to how this happens. It’s not bad luck. It’s not just genetics. It’s decades of eating more than your body can handle, moving less, and sleeping poorly. Processed carbs, sugary drinks, and constant snacking keep insulin levels high. Your cells get numb to it. Over time, inflammation sets in. Fat cells swell. Muscle cells stop taking in glucose. Your liver starts making its own sugar, even when you haven’t eaten.
The good news? You can reverse this - at least for a while. The Diabetes Prevention Program (DPP) showed that people with prediabetes and metabolic syndrome who lost just 7% of their body weight and walked 150 minutes a week cut their risk of diabetes by 58%. That’s more effective than metformin, the standard drug for prediabetes, which reduces risk by 31%. Lifestyle isn’t a backup plan - it’s the first line of defense.
Real people see results. One man in Melbourne, 52, was diagnosed with metabolic syndrome in 2023. His waist was 102 cm, triglycerides 210, fasting glucose 112. He started walking 30 minutes after dinner, swapped soda for sparkling water, and cut out late-night snacks. In six months, his waist dropped to 90 cm, triglycerides fell to 110, and glucose normalized. He didn’t need medication. He didn’t even feel like he was dieting - he just changed his habits.
Medications That Help - But Don’t Fix
Metformin is still the go-to drug for prediabetes. It helps the liver make less glucose and makes muscle cells more sensitive to insulin. But it doesn’t reverse fat buildup or inflammation. Newer drugs like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro) are changing the game. In clinical trials, semaglutide led to nearly 15% weight loss over a year. Tirzepatide, which targets two hormones instead of one, helped 66% of patients achieve diabetes remission - meaning their blood sugar returned to normal without meds.
But these aren’t magic pills. They work best when paired with diet and movement. Stop the lifestyle changes, and the weight comes back. The drugs are tools - not replacements. And they’re expensive. Most insurance won’t cover them unless you already have diabetes or severe obesity.

What to Watch For - And When to Act
Most people with insulin resistance feel fine. That’s why it’s called silent. But there are clues:
- Constant hunger, even after eating
- Cravings for carbs and sugar
- Feeling tired after meals
- Difficulty losing weight, especially around the middle
- Dark patches on skin - neck, armpits, groin (acanthosis nigricans)
If you have two or more of these, get checked. Ask for a fasting glucose test, an HbA1c (which shows average blood sugar over 3 months), and a lipid panel. If your HbA1c is 5.7-6.4%, you’re in prediabetes. That’s your wake-up call.
And don’t wait for a diagnosis to start. Start walking. Cut out sugary drinks. Eat protein and fiber at every meal. Sleep 7-8 hours. Reduce stress. These aren’t “lifestyle changes” - they’re survival tools.
What Comes Next - And How to Stay Ahead
Research is moving fast. In 2024, Vertex Pharmaceuticals showed that stem-cell-derived beta cells could restore insulin production in type 2 diabetes patients - 71% of participants reached normal HbA1c without insulin after one year. That’s not a cure yet, but it’s a glimpse of what’s possible.
Continuous glucose monitors (CGMs) are no longer just for diabetics. The Dexcom G7, approved in late 2023, lets you see how your meals, sleep, and stress affect your blood sugar in real time. Many people with prediabetes use them to learn what foods spike their glucose - and what doesn’t. It turns guesswork into data.
The big picture? By 2050, 1 in 3 Americans could have diabetes. The cost? Over $1 trillion a year in the U.S. alone. But the Lancet Commission says we can cut new cases by 40-60% by 2035 - if we act now. Policy changes matter: taxing sugary drinks, making healthy food cheaper, building walkable cities. But your daily choices matter more.
Insulin resistance isn’t your fault. But reversing it? That’s your power.
Is insulin resistance the same as type 2 diabetes?
No. Insulin resistance is the underlying problem that usually comes first. Type 2 diabetes happens when your pancreas can no longer make enough insulin to overcome that resistance. You can have insulin resistance for years without having diabetes. That’s why checking for it early matters.
Can you reverse metabolic syndrome?
Yes - especially in the early stages. Losing 5-7% of your body weight, getting 150 minutes of walking or similar activity each week, and cutting out added sugar and refined carbs can normalize blood pressure, triglycerides, and glucose levels. Studies show that 30-50% of people with metabolic syndrome can reverse it within a year with consistent lifestyle changes.
Do I need medication if I have insulin resistance?
Not always. Many people reverse insulin resistance with diet, movement, and sleep alone. But if your fasting glucose is above 100 mg/dL and you’re at high risk for diabetes - especially if you’re overweight or have a family history - your doctor may recommend metformin. It’s not a cure, but it buys you time and reduces your risk by about one-third.
Why does my doctor care about my waist size?
Because belly fat is metabolically active. Unlike fat under your skin, visceral fat releases inflammatory chemicals and fatty acids directly into your liver. That’s what drives insulin resistance, high triglycerides, and high blood pressure. Waist size is a better predictor of metabolic risk than BMI.
Can I have metabolic syndrome and not be overweight?
Yes. People with a normal BMI can still have high visceral fat and insulin resistance - especially those with South Asian, Hispanic, or Indigenous ancestry. This is sometimes called "TOFI" - thin outside, fat inside. A waist measurement above 90 cm for men or 80 cm for women is a red flag, regardless of your weight.
What’s the best way to check for insulin resistance?
There’s no single perfect test. Doctors usually look at a combination: fasting glucose, HbA1c, triglycerides, HDL, blood pressure, and waist size. A high triglyceride-to-HDL ratio (above 3.5) is a strong clue. Some clinics offer an HOMA-IR test, which calculates insulin resistance from fasting insulin and glucose levels - but it’s not widely available. If you have three of the five metabolic syndrome criteria, you’re almost certainly insulin resistant.
Next Steps: What to Do Today
Don’t wait for a diagnosis. If you’re over 40, overweight, or have a family history of diabetes, get tested. Even if you feel fine, your body might be sending signals you’re ignoring.
- Get your fasting glucose and HbA1c checked - ask your doctor.
- Measure your waist - stand, breathe out, and wrap a tape around your belly at the level of your navel.
- Swap one sugary drink a day for water, tea, or sparkling water.
- Walk for 20 minutes after dinner - three times this week.
- Write down what you eat for two days. Look for hidden sugars - sauces, bread, yogurt, granola bars.
You don’t need to overhaul your life overnight. Small, consistent changes add up. And if you act now - before your pancreas gives out - you might never need medication at all.

Vincent Soldja
December 3, 2025 AT 01:41Albert Essel
December 4, 2025 AT 08:54Charles Moore
December 5, 2025 AT 00:44Gavin Boyne
December 6, 2025 AT 22:47Rashi Taliyan
December 8, 2025 AT 21:28Kara Bysterbusch
December 9, 2025 AT 15:54Rashmin Patel
December 10, 2025 AT 19:04sagar bhute
December 12, 2025 AT 07:13Cindy Lopez
December 13, 2025 AT 22:03shalini vaishnav
December 15, 2025 AT 01:13vinoth kumar
December 16, 2025 AT 12:18bobby chandra
December 17, 2025 AT 11:39Archie singh
December 19, 2025 AT 09:47Gene Linetsky
December 21, 2025 AT 01:27Ignacio Pacheco
December 21, 2025 AT 17:03