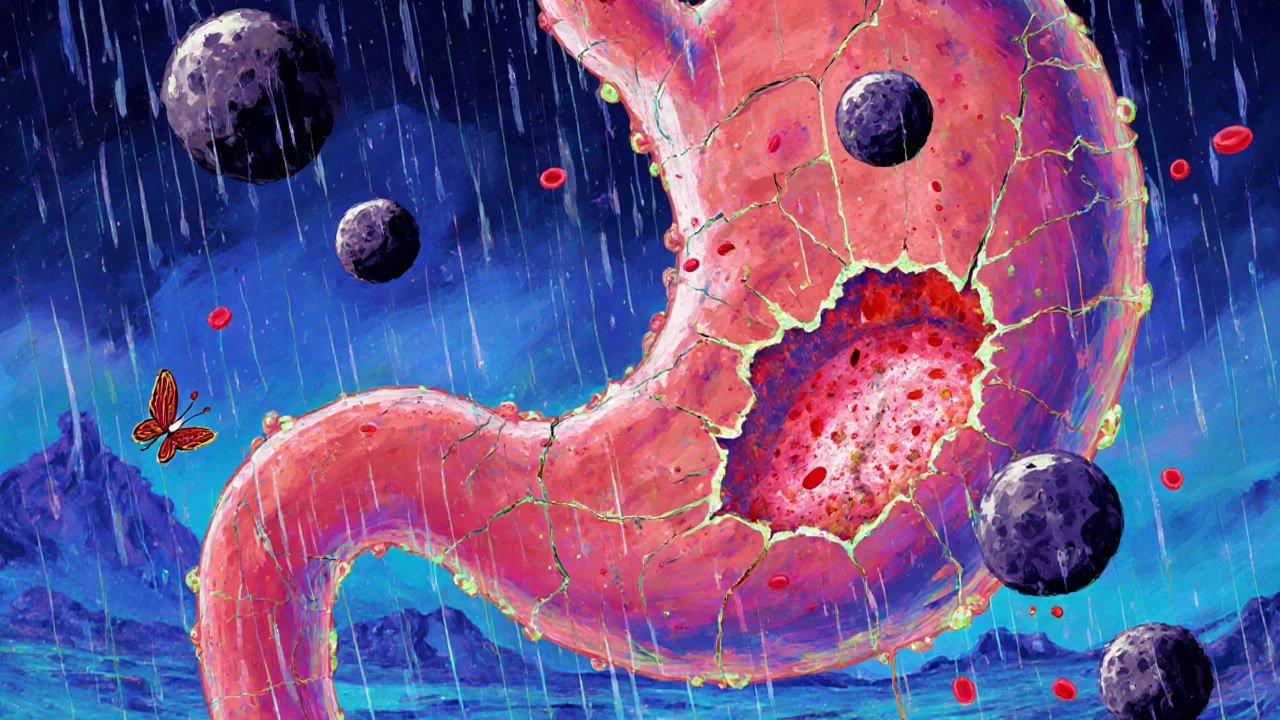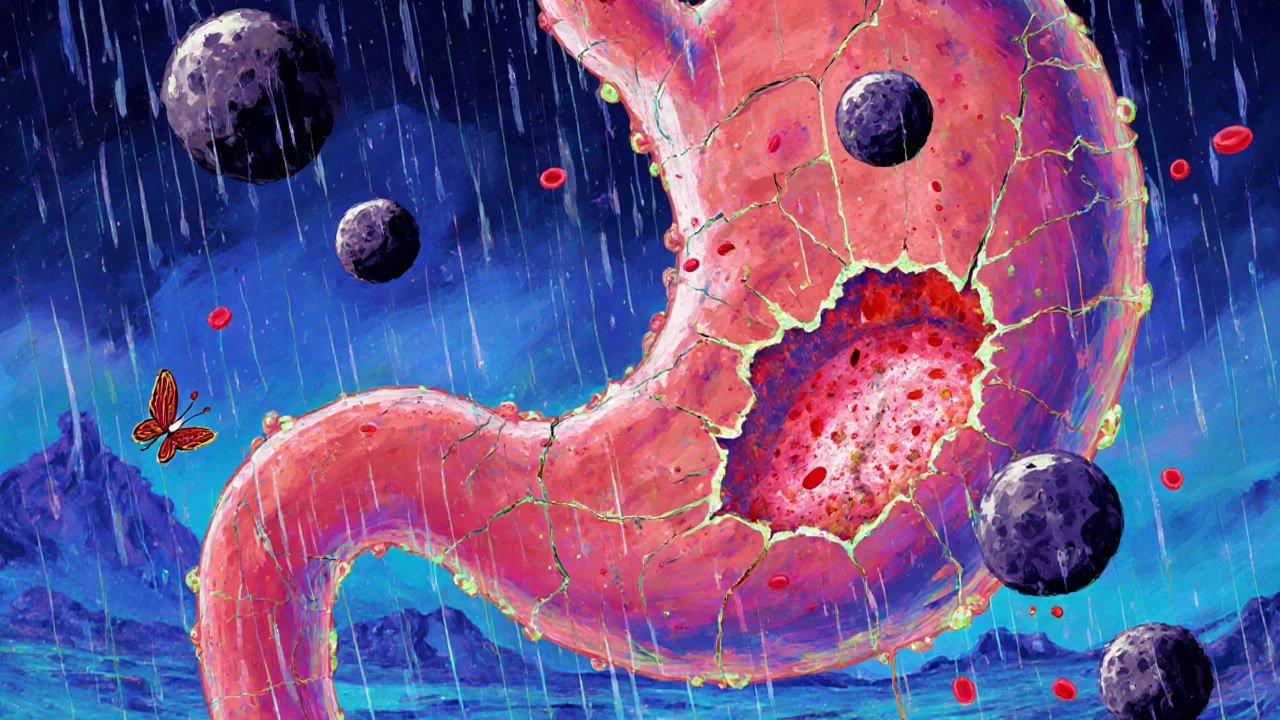
Peptic Ulcer: Causes, Treatments, and What You Need to Know
When your stomach lining gets damaged and forms an open sore, you’re dealing with a peptic ulcer, a break in the lining of the stomach, duodenum, or esophagus caused by acid and enzymes. Also known as a stomach ulcer, it’s not just discomfort—it’s a sign something deeper is off. Many people think stress or spicy food causes it, but the real culprits are usually H. pylori, a bacterium that weakens the protective mucus layer in the gut or long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs), like ibuprofen or aspirin, which block the body’s natural stomach protection. These two factors alone account for over 90% of cases.
Left untreated, a peptic ulcer doesn’t just hurt—it can bleed, perforate, or block your digestive tract. That’s why recognizing the signs matters: burning pain between meals or at night, bloating, nausea, and sometimes vomiting or black stools. It’s not always obvious, and some people have no symptoms until something serious happens. The good news? Most ulcers heal quickly once you know what’s causing them. Treatment usually involves killing H. pylori with antibiotics, reducing acid with proton pump inhibitors, medications like omeprazole that shut down acid production at the source, and avoiding triggers like smoking, alcohol, and NSAIDs. Even if you feel better after a few days, finishing the full course of treatment is critical—H. pylori can come back if you don’t.
Some people also have gastritis, inflammation of the stomach lining that often overlaps with ulcers and shares the same root causes. The line between the two can be blurry, but both respond to similar strategies. Lifestyle changes—eating smaller meals, not lying down right after eating, cutting back on caffeine—help reduce irritation. And while stress doesn’t cause ulcers, it can make symptoms worse by increasing acid and slowing healing.
What you’ll find below is a collection of real, practical guides that connect directly to peptic ulcer care. You’ll see how certain medications interact with other drugs, what alternatives exist for managing pain without harming your stomach, and how food triggers can mimic or worsen ulcer symptoms. These aren’t theoretical articles—they’re based on real patient experiences and clinical evidence. Whether you’re trying to understand why your pain won’t go away, or you’re looking for safer ways to manage chronic conditions without triggering ulcers, the posts here give you the clear, no-fluff answers you need.