NSAID Risk Assessment Tool
Assess Your NSAID Risk
This tool helps you understand your risk of gastrointestinal bleeding when taking NSAIDs like ibuprofen or naproxen. Based on your health factors, you'll get a personalized risk level and recommendations.
Your Risk Assessment
Every year, millions of people reach for ibuprofen, naproxen, or aspirin to ease a headache, back pain, or arthritic flare-up. These drugs - called NSAIDs - work fast and they work well. But for many, the relief comes with a hidden cost: gastrointestinal bleeding. It’s not rare. It’s not theoretical. It’s happening right now to people who never thought a painkiller could hurt them.
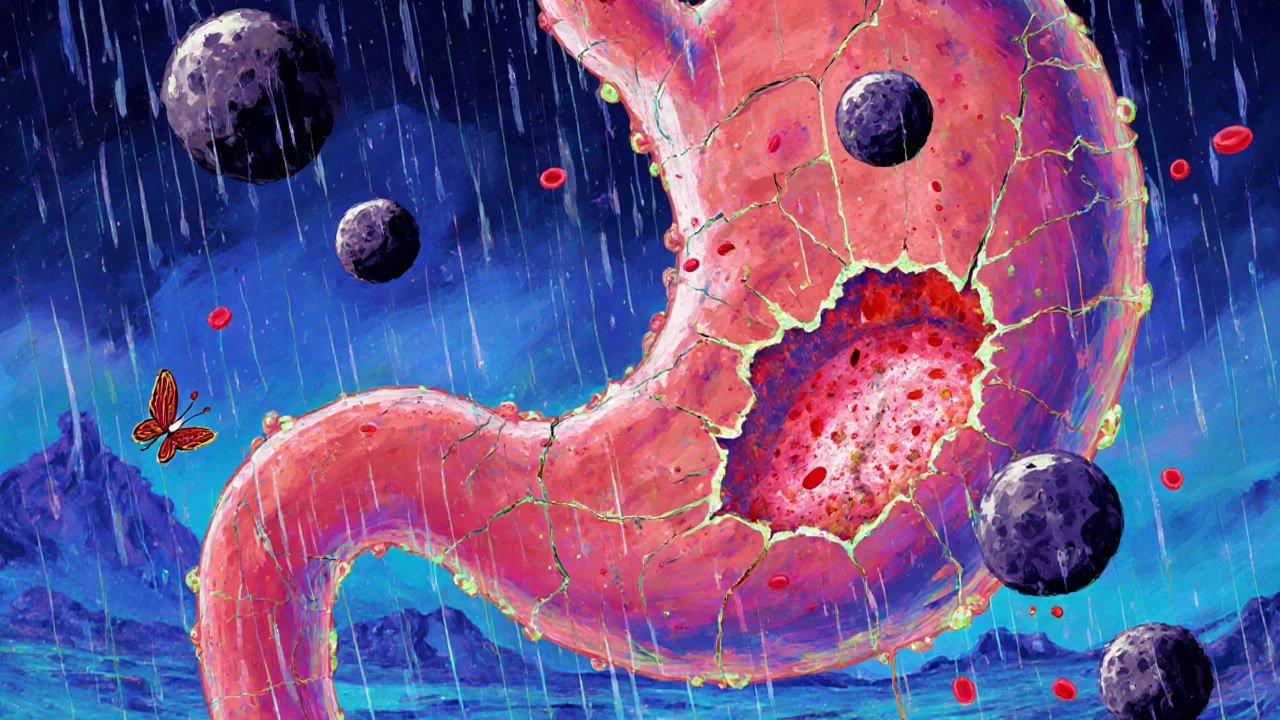
How NSAIDs Cause Ulcers and Bleeding
NSAIDs don’t just block pain signals. They shut down enzymes in your body called COX-1 and COX-2. COX-2 is involved in inflammation - that’s why these drugs help with swelling and joint pain. But COX-1? That’s the enzyme that keeps your stomach lining protected. It helps make mucus and bicarbonate, the natural shield that keeps stomach acid from eating away at your own tissue. When you take an NSAID, especially long-term or at high doses, you’re stripping away that shield. Without it, stomach acid starts damaging the lining. At first, it’s just tiny erosions - barely noticeable. But over time, those can turn into deep ulcers. And when an ulcer cuts into a blood vessel? That’s when bleeding starts. This isn’t just about stomach pain. Many people don’t feel anything until it’s too late. Bleeding can be slow and hidden - causing iron deficiency anemia, fatigue, or dizziness. Or it can be sudden and severe: black, tarry stools, vomiting blood, or fainting. A 2020 meta-analysis found NSAID users are 3 to 4 times more likely to suffer upper GI bleeding than non-users. And in nearly one-third of cases, the bleeding comes from the lower intestine - not the stomach at all.Who’s at the Highest Risk?
Not everyone who takes NSAIDs will bleed. But some people are walking into danger without knowing it.- People over 65 - risk doubles with every decade past 60
- Those with a past history of ulcers - their chance of bleeding again jumps by 2.5 times
- Anyone taking blood thinners like warfarin or aspirin - that combination raises bleeding risk by more than double
- People using corticosteroids (like prednisone) along with NSAIDs - another 80% increase in risk
- Those taking multiple NSAIDs at once - even mixing prescription and OTC versions
- Patients on high doses - over 1,200 mg of ibuprofen daily
Not All NSAIDs Are Created Equal
You might think all painkillers are the same. They’re not. Traditional NSAIDs - like ibuprofen, naproxen, and diclofenac - block both COX-1 and COX-2. That’s why they’re more likely to cause ulcers. In contrast, COX-2 inhibitors like celecoxib (Celebrex) were designed to spare the stomach. A landmark 2000 Lancet study showed celecoxib caused about half as many serious ulcers as ibuprofen. But here’s the catch: COX-2 inhibitors raise heart attack and stroke risk. Rofecoxib (Vioxx) was pulled off the market in 2004 after studies showed it nearly doubled heart attack risk. Celecoxib still carries a warning, though its risk is lower than rofecoxib’s. So choosing between them isn’t just about your stomach - it’s about your heart too. For someone with arthritis and a history of ulcers, a COX-2 inhibitor might be safer. For someone with heart disease, a traditional NSAID with a stomach protector might be better.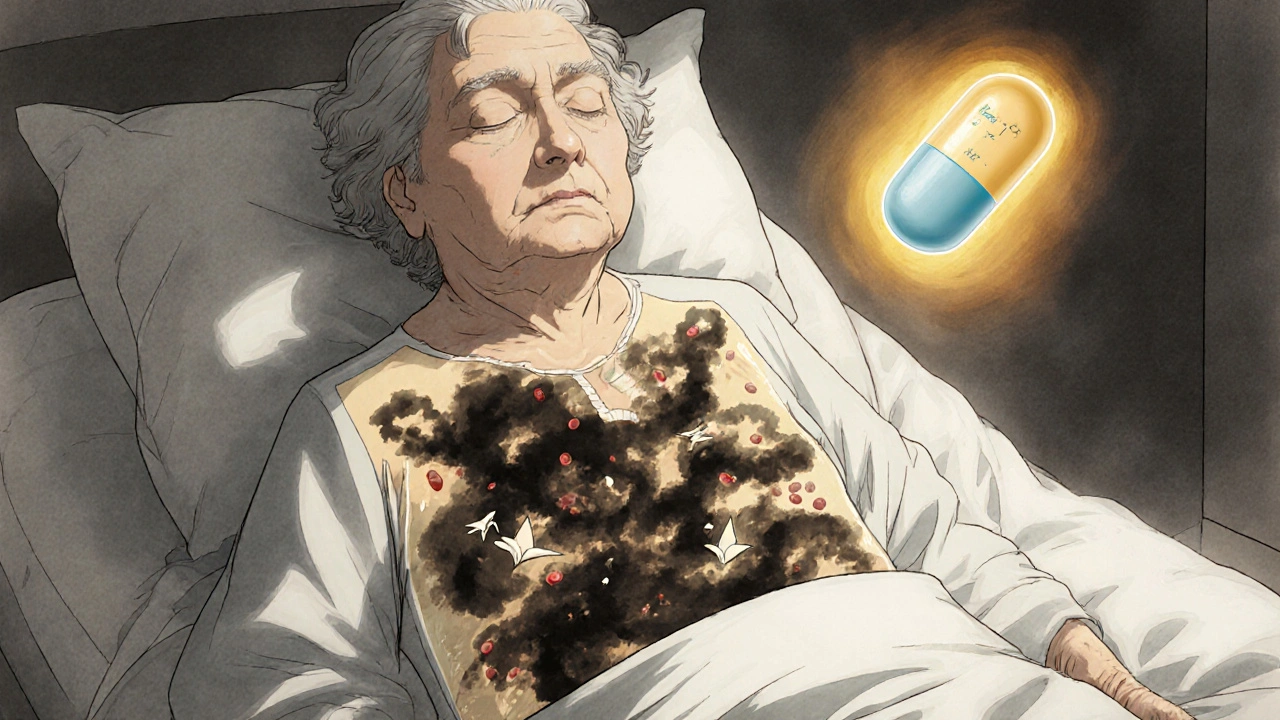
How to Protect Your Stomach
If you need NSAIDs and you’re at risk, you don’t have to go without pain relief. You just need protection. The gold standard is adding a proton pump inhibitor (PPI). These drugs - like omeprazole, esomeprazole, or pantoprazole - cut stomach acid production by up to 90%. A 2017 Cochrane review of over 13,000 patients found PPIs reduce NSAID-related ulcers by 75%. That’s not a small benefit. That’s life-saving. There’s also misoprostol, a drug that rebuilds the stomach lining. It works almost as well as PPIs - but it causes diarrhea in up to 20% of users and can trigger uterine contractions, so it’s not safe for pregnant women. Newer options are emerging. In 2023, the FDA approved Vimovo - a single pill that combines naproxen with esomeprazole. In a 2022 trial, it cut ulcer complications from 25.6% down to just 7.3% compared to naproxen alone.What Patients Are Really Experiencing
Behind the statistics are real people. On Reddit, a caregiver shared how their 78-year-old mother ended up in the ER needing three blood transfusions. She’d been taking ibuprofen daily for knee pain. No stomach issues. No warning. Just fatigue - which everyone assumed was aging. By the time they tested her iron levels, she was critically anemic. On HealthUnlocked, 63% of people who took NSAIDs reported stomach discomfort. But only 37% told their doctor. Why? Many think it’s normal. Or they don’t want to stop their pain relief. Or they don’t know it’s dangerous. Meanwhile, on Drugs.com, 78% of celecoxib users reported no GI problems. But 42% of people on traditional NSAIDs quit because of nausea, bloating, or bleeding. That’s nearly half of users - not because the drug didn’t work, but because their body couldn’t handle it.
What Doctors Should Do - and What You Should Ask
Doctors aren’t always checking for this. A 2020 study found that over-the-counter NSAID use is often missed during medical visits. People don’t mention it. Doctors don’t ask. If you’re over 60, have a history of ulcers, or take blood thinners - ask your doctor: “Am I at risk for bleeding from this painkiller?” If you’re on NSAIDs long-term, ask: “Do I need a stomach protector?” Don’t assume OTC means safe. Taking two 200 mg ibuprofen tablets four times a day is 1,600 mg - way above the recommended daily limit. And if you’re taking Tylenol for pain on top of that? That’s fine. But if you’re also taking Advil, Aleve, or aspirin? That’s where things get dangerous.The Bigger Picture
NSAIDs cause about 107,000 hospitalizations and 16,500 deaths every year in the U.S. alone. The cost? Over $2 billion annually. And yet, they’re still among the most prescribed drugs in the world. Why? Because they work. Arthritis, back pain, headaches - they’re common. And for many, there’s no better option. The goal isn’t to stop NSAIDs. It’s to use them smarter. The American College of Rheumatology now recommends: for people with one risk factor, use the lowest dose for the shortest time. For two or more risk factors - use a COX-2 inhibitor with a PPI. That’s the safest path forward. Future drugs are coming. Trials are underway for CINODs - new NSAIDs that release nitric oxide to protect the stomach. Early results show 50% fewer ulcers than naproxen. But they’re still years away. For now, the answer is simple: know your risk. Talk to your doctor. Don’t ignore stomach symptoms. And if you’re at risk - take the PPI. It’s not extra. It’s essential.Can I take ibuprofen if I’ve had a stomach ulcer before?
If you’ve had a peptic ulcer or GI bleeding in the past, taking ibuprofen or other NSAIDs without protection is dangerous. Your risk of bleeding again is over 2.5 times higher. If you must use an NSAID, combine it with a proton pump inhibitor (PPI) like omeprazole, or use a COX-2 inhibitor like celecoxib with a PPI. Never take NSAIDs alone after a prior ulcer.
Do all NSAIDs cause bleeding?
All NSAIDs carry some risk, but not equally. Non-selective NSAIDs like naproxen, diclofenac, and ibuprofen are more likely to cause ulcers and bleeding because they block COX-1, which protects the stomach lining. Selective COX-2 inhibitors like celecoxib have lower GI risk - but higher heart risk. Even low-dose aspirin, often thought of as safe, increases bleeding risk in people with ulcers.
How do I know if NSAIDs are causing internal bleeding?
Signs aren’t always obvious. Overt bleeding means black, tarry stools or vomiting blood - that’s urgent. But occult bleeding is silent: unexplained fatigue, shortness of breath, pale skin, or dizziness. These can mean you’re losing blood slowly, leading to iron deficiency anemia. A simple blood test can check your hemoglobin and iron levels. If you’re on long-term NSAIDs and feel unusually tired, get tested.
Is it safe to take NSAIDs occasionally, like once a week?
For healthy people under 60 with no history of ulcers or heart disease, occasional use (once or twice a week) is generally low risk. But if you’re over 65, take blood thinners, or have kidney disease, even occasional use can be risky. There’s no safe threshold for everyone - it depends on your personal risk profile. Always talk to your doctor before using NSAIDs regularly, even if it’s just for a headache.
Can I just take antacids instead of a PPI to protect my stomach?
Antacids like Tums or Maalox may help with heartburn, but they don’t prevent NSAID-induced ulcers. They neutralize acid temporarily, but don’t reduce acid production like PPIs do. Studies show antacids have no meaningful effect on reducing bleeding risk from NSAIDs. If you need protection, use a PPI - not an antacid.
What are the side effects of PPIs?
PPIs are generally safe for short-term use. Long-term use (over a year) may slightly increase the risk of bone fractures, low magnesium levels, or certain infections like C. diff. But for people at high risk of bleeding from NSAIDs, the benefits far outweigh the risks. If you’re on a PPI long-term, ask your doctor about periodic review and whether you still need it.
Brierly Davis
November 5, 2025 AT 16:44Man, I had no idea ibuprofen could do this to you. My grandma took it daily for her knees and ended up in the ER last year. No warning, just super tired and pale. Doc said she was anemic as hell. Now she’s on omeprazole with her pain meds and feels like a new person. Seriously, if you’re over 60 and popping NSAIDs like candy, talk to your doctor. It’s not worth the risk.
Also, PPIs aren’t scary. They’re lifesavers. Stop treating them like some evil magic potion.
Amber O'Sullivan
November 5, 2025 AT 19:24Jim Oliver
November 7, 2025 AT 01:32William Priest
November 8, 2025 AT 00:43Ryan Masuga
November 9, 2025 AT 05:40Jennifer Bedrosian
November 11, 2025 AT 01:04Lashonda Rene
November 11, 2025 AT 18:23Andy Slack
November 12, 2025 AT 09:09