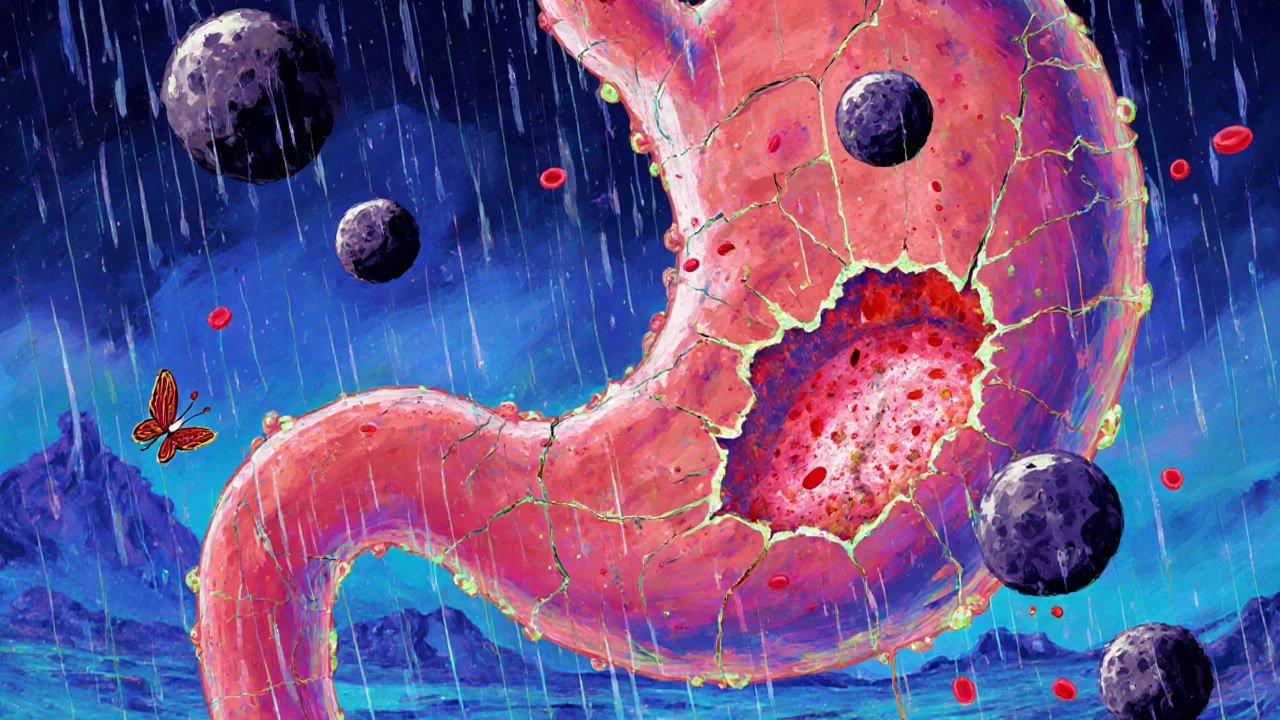
Gastrointestinal Bleeding: Causes, Signs, and What to Do Next
When you're dealing with gastrointestinal bleeding, a loss of blood from any part of the digestive tract, from the esophagus to the rectum. Also known as GI bleeding, it’s not a disease on its own—it’s a symptom that something else is wrong inside your gut. This isn’t something to ignore. Even a small amount of blood in your stool or vomit can mean a serious issue like an ulcer, a torn blood vessel, or inflammation from conditions like Crohn’s or diverticulitis.
People often mistake GI bleeding for something mild—like hemorrhoids or a bad stomach bug. But if you’re seeing dark, tarry stools, bright red blood in your poop, or vomiting material that looks like coffee grounds, that’s your body screaming for help. peptic ulcers, open sores in the stomach or upper small intestine, often caused by H. pylori bacteria or long-term NSAID use are one of the most common reasons. esophageal varices, swollen veins in the esophagus linked to liver disease are another major cause, especially in those with chronic alcohol use or hepatitis. And while diverticulosis, small pouches in the colon wall that can bleed without warning is more common in older adults, it can strike anyone.
What makes this tricky is that some people don’t feel pain at all. You might just feel tired, dizzy, or short of breath—signs your body is low on iron and oxygen. That’s why it’s easy to delay seeing a doctor. But the faster you get checked, the better your chances of stopping the bleed before it becomes life-threatening. Treatment can range from simple meds to endoscopic procedures, depending on where and how bad the bleed is. The key is recognizing the red flags early.
Below, you’ll find real-world guides from people who’ve dealt with similar issues—whether it’s understanding how medications like NSAIDs can trigger bleeding, spotting hidden signs of internal blood loss, or learning how conditions like liver disease and autoimmune disorders connect to gut health. These aren’t just theory—they’re practical insights from those who’ve been there.