Drug Hypersensitivity: Signs, Risks, and What to Do When Your Body Reacts
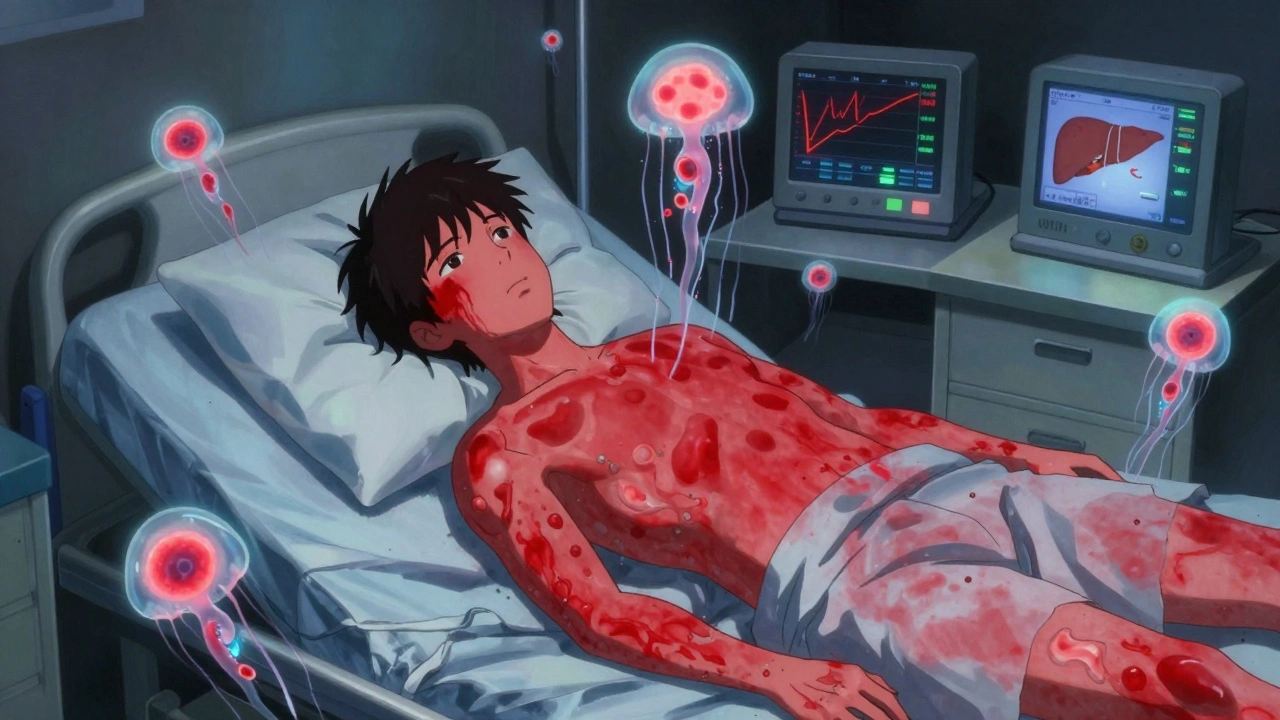
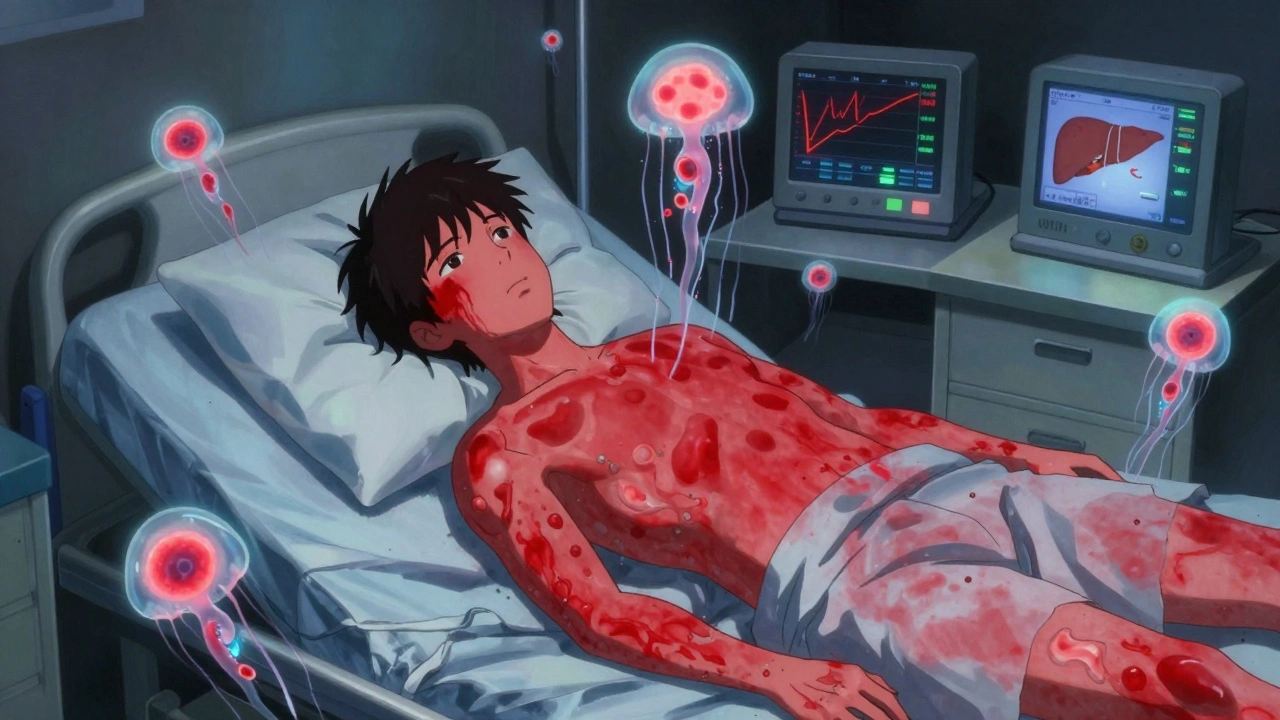
When your body sees a medicine as an invader, it doesn’t just ignore it—it fights back. That’s drug hypersensitivity, an immune system overreaction to a medication that can range from a rash to life-threatening shock. Also known as allergic reaction to medication, it’s not just about itching or hives—it’s your body’s warning system going off, even when the drug is meant to help. Unlike side effects, which are predictable and common, drug hypersensitivity is unpredictable and personal. One person takes amoxicillin and feels fine. Another breaks out in blisters. There’s no way to know until it happens.
This isn’t rare. Up to 10% of people will have some kind of reaction to a drug in their lifetime. And it’s not just antibiotics. Painkillers like ibuprofen, seizure meds like phenytoin, and even insulin can trigger it. phenytoin, a drug with a narrow therapeutic window, is especially risky for hypersensitivity reactions in certain populations. The same goes for NSAIDs, common over-the-counter pain relievers that can cause severe skin reactions or breathing trouble in sensitive individuals. If you’ve ever had a rash after taking a new pill, or felt your throat close up after a shot, you’ve seen drug hypersensitivity in action.
What makes it dangerous is how fast it can escalate. A mild rash today could turn into Stevens-Johnson syndrome tomorrow—where skin starts peeling off like a burn. Or it could trigger anaphylaxis, a full-body crash that needs emergency treatment. And here’s the catch: once your body reacts to a drug, it usually remembers. Next time you take it—even years later—the reaction can be worse. That’s why knowing your triggers matters more than you think.
Some people are more at risk. If you have a history of allergies, autoimmune diseases, or HIV, your chances go up. Certain genetic markers also make reactions more likely, especially with drugs like carbamazepine or allopurinol. But you don’t need a lab test to spot the warning signs. Pay attention: Did a new medication come with unexplained fever? A swollen face? Blisters in your mouth? These aren’t "just side effects"—they’re red flags.
And here’s something most people miss: drug hypersensitivity isn’t always immediate. Sometimes it shows up days or weeks after you start a new medicine. That’s why it’s easy to blame something else—like a virus or stress. But if you’re feeling off after starting a new pill, don’t brush it off. Write down what you took, when, and what happened. That record could save your life next time.
The good news? You can avoid most of these reactions. If you’ve had one before, tell every doctor and pharmacist. Keep a list. Don’t assume a generic version is safe—it’s the same active ingredient. And if you’re unsure, ask: "Could this cause an allergic reaction?" Most people don’t, but you should. Your body already gave you the signal. Now it’s time to listen.
Below, you’ll find real stories and science-backed advice on how to recognize, avoid, and manage these reactions. From how coffee interferes with thyroid meds to why liquid antibiotics expire fast, these posts don’t just explain what’s happening—they show you how to stay safe.