Diabetic Kidney Disease: Causes, Signs, and How Medications Help
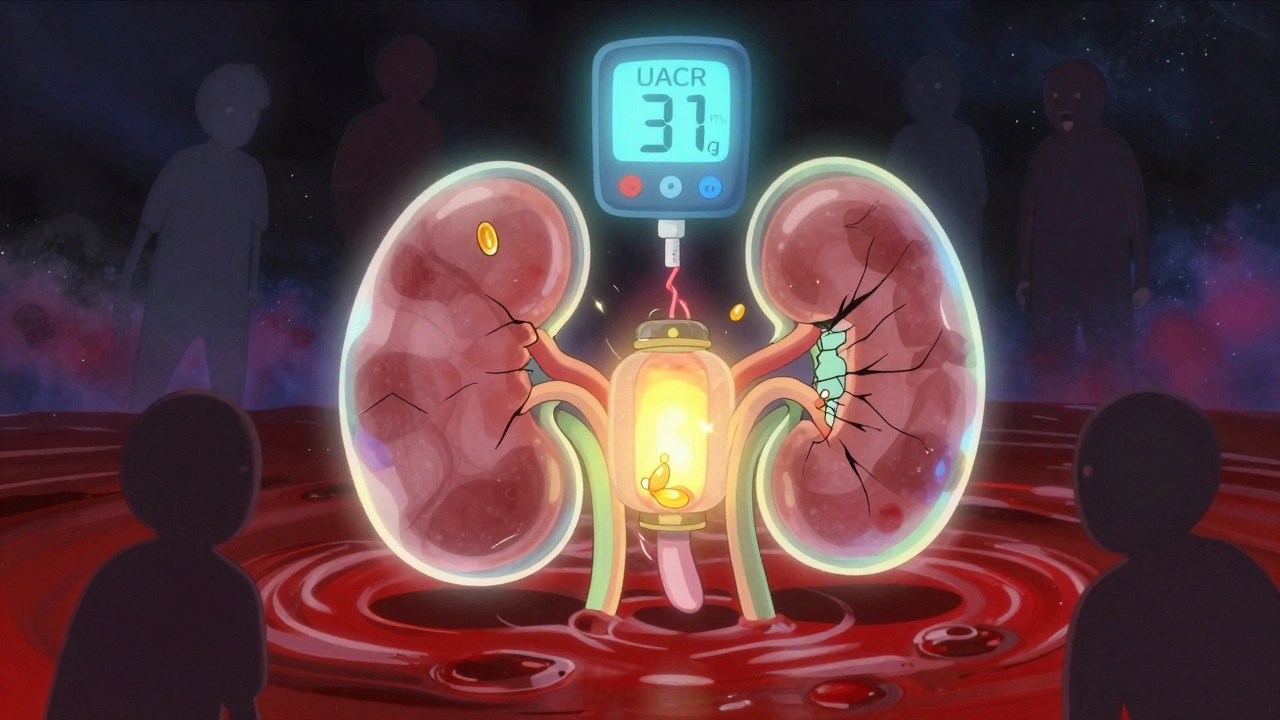
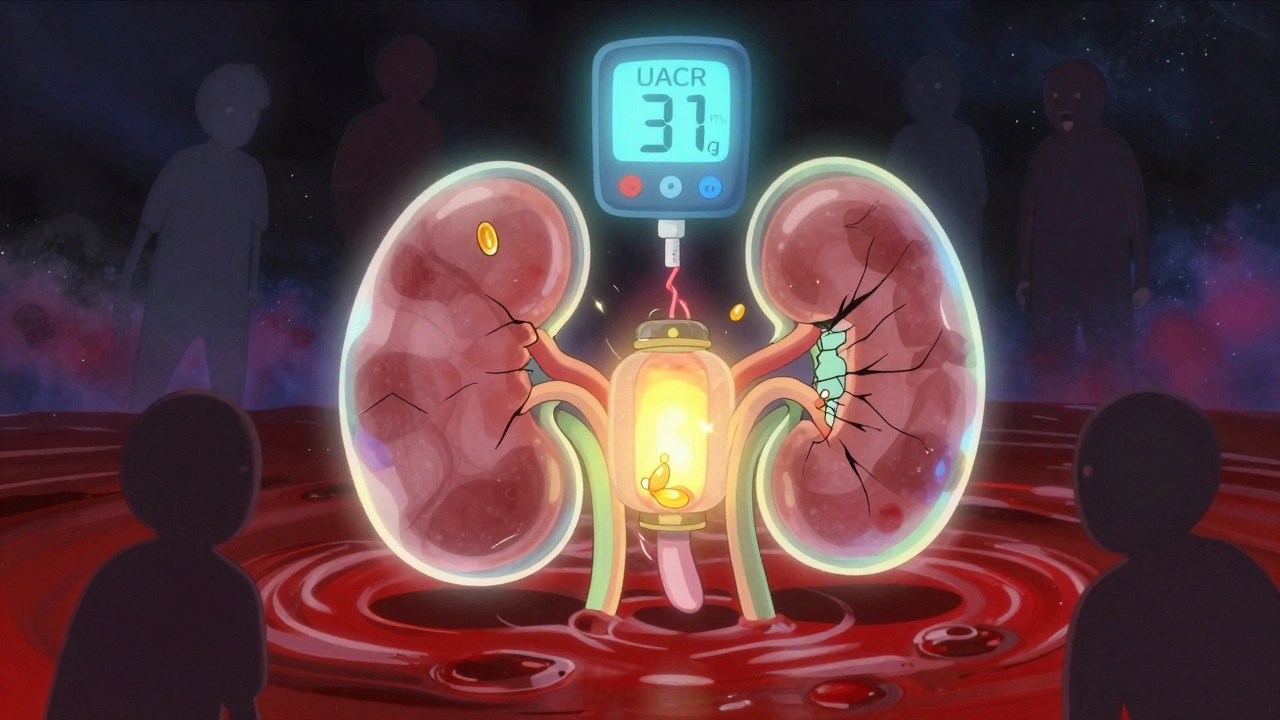
When you have diabetic kidney disease, a progressive condition where high blood sugar damages the tiny filters in your kidneys. Also known as diabetic nephropathy, it’s one of the most common reasons people with diabetes end up on dialysis. This isn’t just about sugar levels—it’s about how that sugar quietly tears down your body’s natural filtration system over years. Your kidneys don’t just remove waste—they balance fluids, control blood pressure, and help make red blood cells. When they start failing because of diabetes, everything else starts to slip.
Blood sugar control, the foundation of managing diabetes, is the first line of defense. But even with good numbers, some people still develop kidney damage. That’s because high glucose doesn’t just float around—it sticks to proteins, triggers inflammation, and squeezes blood vessels in the kidneys. Over time, this leads to protein leaking into urine, swelling in legs, rising blood pressure, and eventually, reduced kidney function. Kidney health medications, like ACE inhibitors and SGLT2 inhibitors, aren’t just for lowering blood pressure—they actively protect the kidneys by reducing pressure inside the filtering units and helping the body get rid of excess sugar through urine.
What’s surprising is that many people don’t feel anything until the damage is advanced. No pain. No warning. Just a slow decline. That’s why regular urine and blood tests are non-negotiable if you have diabetes. The same drugs that help with heart risks in diabetes—like empagliflozin or lisinopril—are now proven to delay kidney failure. And it’s not just pills. Diet, hydration, and avoiding NSAIDs like ibuprofen (which you’ll see discussed in other posts) play a big role too. This isn’t a one-time fix. It’s a daily, long-term game of prevention.
Below are real-world insights from posts that cover how medications work, how to avoid harmful interactions, and what actually helps when your kidneys are under stress from diabetes. You’ll find practical advice on drug safety, how to monitor your condition, and what to ask your doctor—not just theory, but what works in daily life.