When you hear the word polysomnography, it might sound like something out of a sci-fi movie. But in reality, it’s just the medical term for a sleep study - a test millions of people have undergone to find out why they’re tired all the time, snore loudly, or wake up gasping for air. If you’ve been told you need one, you’re probably wondering: What happens during the test? Will I be able to sleep? And what do the results actually mean?
What Exactly Is a Polysomnography Test?
Polysomnography, often called PSG, is the most complete way doctors diagnose sleep disorders. Unlike a quick home test that only checks your breathing, a polysomnography records up to 16 different body functions while you sleep. It looks at brain waves, eye movements, muscle activity, heart rhythm, breathing patterns, oxygen levels, and even body position. All of this happens overnight in a sleep center, not a hospital room - think cozy private room, comfortable bed, and a technician watching from another room. The name comes from Greek: "poly" means many, "somno" means sleep, and "graphy" means recording. So, it’s literally a multi-parameter sleep recording. The American Academy of Sleep Medicine says it’s the gold standard because it doesn’t just spot sleep apnea - it can catch narcolepsy, restless legs syndrome, night terrors, and even seizures that happen while you sleep.What Gets Monitored During the Test?
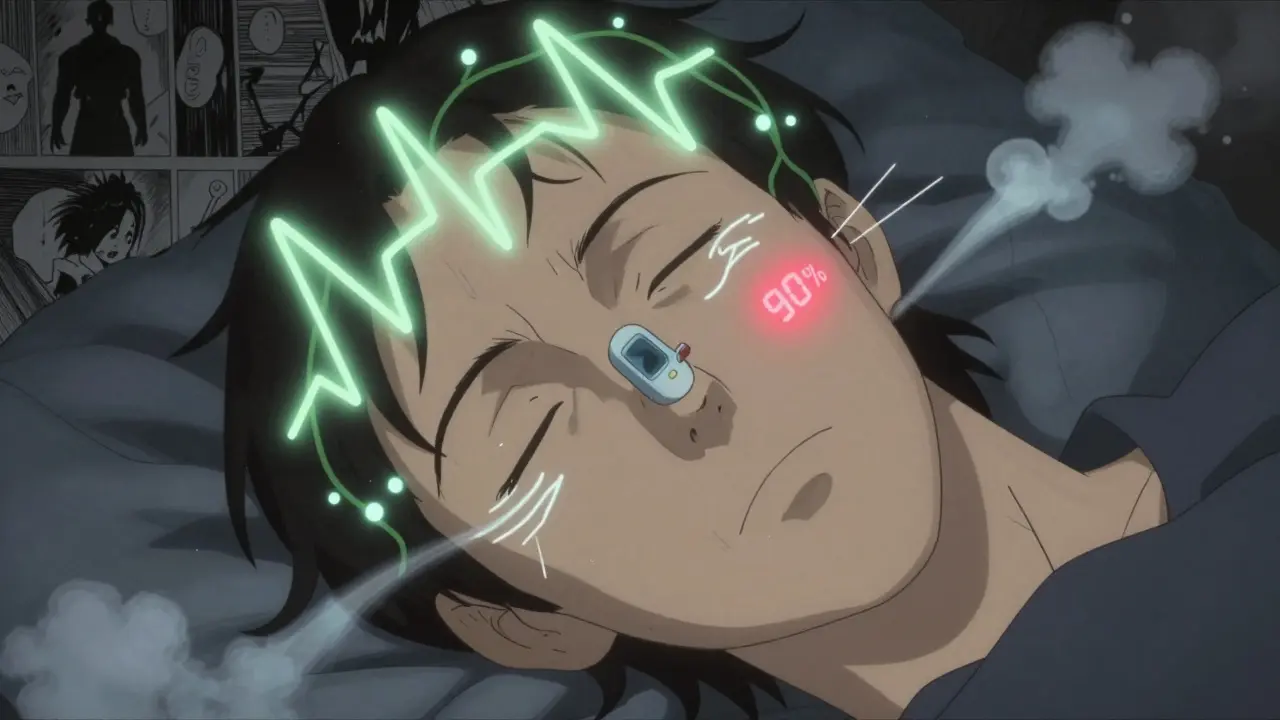
You’ll have about 22 small sensors attached to your skin. No needles. No pain. Just sticky patches and soft bands.- EEG (electroencephalogram): Electrodes on your scalp track brain waves to tell which sleep stage you’re in - light sleep, deep sleep, or REM. This is critical. If you fall into REM sleep too fast, it could mean narcolepsy.
- EOG (electrooculogram): Sensors near your eyes detect rapid eye movements. These only happen during REM sleep, so they help map your sleep cycles.
- EMG (electromyogram): Tiny wires on your chin and legs check muscle tone. If your leg muscles jerk every 30 seconds, it could be restless legs syndrome. If your jaw clenches, it might be bruxism.
- ECG (electrocardiogram): Monitors your heart rate and rhythm. Some sleep disorders cause dangerous heart pauses or irregular beats.
- Respiratory belts: Bands around your chest and stomach track how hard you’re trying to breathe. This helps tell the difference between obstructive sleep apnea (airway blocked but you’re still trying to breathe) and central sleep apnea (your brain stops telling your lungs to breathe).
- Nasal airflow sensors: A small tube under your nose or a pressure sensor in your nostrils measures whether air is moving in and out.
- Pulse oximeter: A clip on your finger checks your blood oxygen levels. If your oxygen drops below 90% for more than 10 seconds, that’s a red flag.
- Body position sensor: Tells if you’re sleeping on your back - a common trigger for snoring and apnea.
- Audio and video: Cameras and microphones record snoring, talking, screaming, or unusual movements. This helps diagnose parasomnias like sleepwalking or REM sleep behavior disorder.
How Is It Different From a Home Sleep Test?
Home sleep apnea tests (HSAT) are cheaper and more convenient. But they only measure 3 to 4 things: airflow, oxygen levels, breathing effort, and heart rate. They’re great if you’re likely to have simple obstructive sleep apnea and have no other symptoms. But if you’re also experiencing daytime fatigue, leg jerks, nightmares, or sudden sleep attacks, a home test won’t cut it. It can’t detect narcolepsy. It can’t tell if you’re having seizures. It can’t measure sleep stages. And about 15-20% of home tests fail because the equipment comes loose or you don’t wear it right. In-lab polysomnography has a failure rate of just 2-5%. That’s because a trained sleep technologist is there to fix sensors if they fall off, adjust the room temperature, or even chat with you if you’re nervous. Plus, if you’re found to have moderate to severe sleep apnea during the first half of the night, the study can switch to a split-night setup - meaning they’ll start your CPAP therapy that same night. No second trip needed.What Should You Do Before the Test?
Preparation matters. You’re not just showing up to sleep - you’re helping get accurate results.- Stick to your normal sleep schedule for at least three days before the test. Don’t try to "catch up" on sleep.
- Avoid caffeine after 2 p.m. the day of the test. That includes coffee, tea, soda, and chocolate.
- Don’t nap in the afternoon. Even a 20-minute power nap can mess up your overnight sleep.
- Wash your hair before you come. No conditioners, gels, or sprays - they interfere with electrode contact.
- Bring your own pillow, pajamas, and toiletries. The more homey it feels, the better you’ll sleep.
- Let the sleep center know if you take regular medications - some sleep aids or antidepressants can affect results.
What’s It Like to Sleep With All Those Sensors?
It’s weird at first. Most people say they feel like a robot or a science experiment. But here’s the thing: you don’t have to sleep perfectly. The goal isn’t to get 8 hours of flawless sleep. It’s to get enough sleep - usually 4-6 hours - for the technologist to see your full sleep cycle. About 85% of people get enough data to make a diagnosis, even if they wake up once or twice. The sleep tech can adjust sensors quietly, turn down the lights, or even dim the video camera if you’re uncomfortable. Many patients say the biggest surprise? They slept better than expected. One woman told her doctor she was convinced she’d be awake all night. Instead, she slept 5 hours and woke up saying, "I didn’t even notice the wires."What Do the Results Show?
After the test, a board-certified sleep doctor spends 2-3 hours analyzing the data. The raw output is over 1,000 pages of graphs and numbers. Here’s what they’re looking for:- Sleep efficiency: How much of your time in bed was actual sleep? Below 85% can indicate insomnia or sleep fragmentation.
- Sleep architecture: Did you cycle through NREM and REM stages normally? People with narcolepsy enter REM within 15 minutes - normal people take 90 minutes.
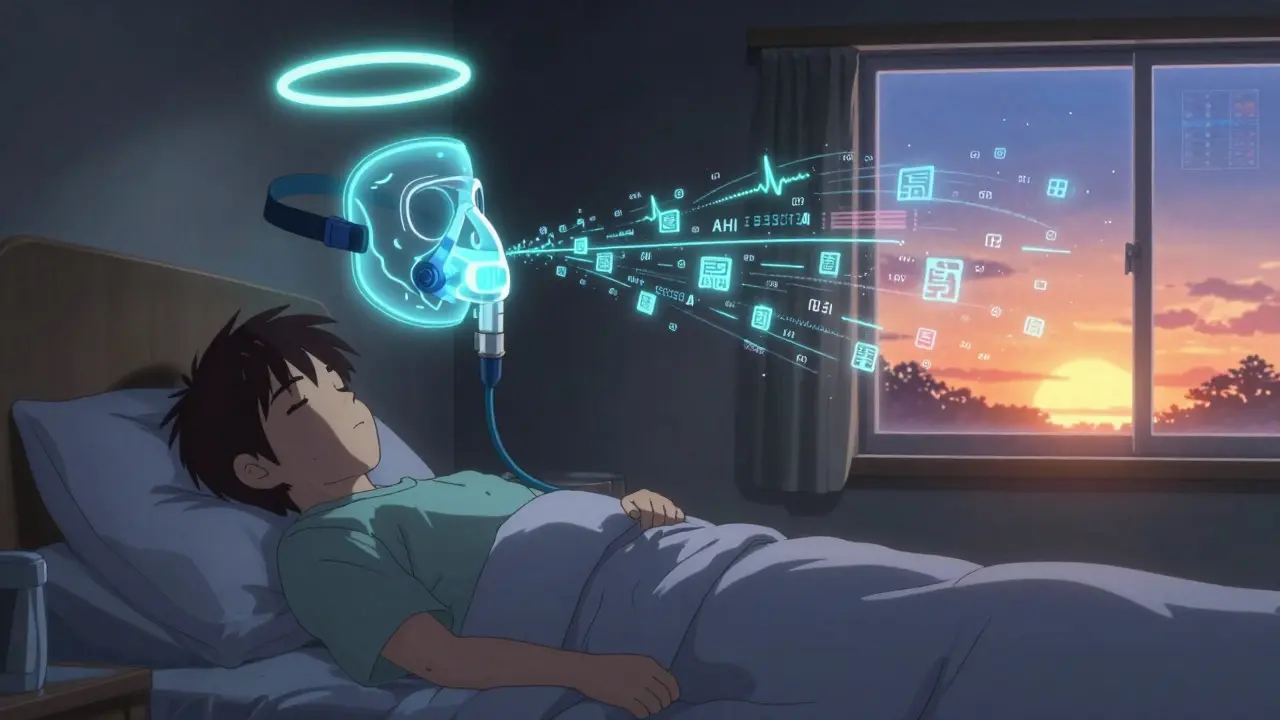
- AHI (Apnea-Hypopnea Index): This is the big one for sleep apnea. It counts how many times you stop or partially stop breathing per hour. AHI of 5-15 = mild, 15-30 = moderate, over 30 = severe.
- Oxygen desaturation: How low did your blood oxygen drop? Drops below 90% for more than 10 seconds are concerning.
- Leg movements: More than 5 leg jerks per hour can signal restless legs syndrome.
- Abnormal behaviors: Screaming, punching, or getting out of bed? That’s REM sleep behavior disorder - and it’s treatable.
What Happens After the Results?
You’ll get a detailed report, usually within 1-2 weeks. Your doctor will explain what it means and what comes next.- If you have sleep apnea: You’ll likely be prescribed CPAP therapy. In a split-night study, you might already have your pressure settings.
- If you have narcolepsy: You may need a second test called MSLT (Multiple Sleep Latency Test) to confirm.
- If you have parasomnias: Medication, safety changes, or behavioral therapy may be recommended.
- If results are normal: Your doctor will look at other causes - depression, anxiety, thyroid issues, or even poor sleep habits.
Insurance and Cost
Most insurance plans, including Medicare, cover polysomnography if you have documented symptoms like loud snoring, witnessed apneas, or excessive daytime sleepiness. Medicare covers 80% of the cost when ordered by a doctor for diagnostic purposes. Private insurers usually require prior authorization. In-lab studies cost between $500 and $3,000, depending on location and whether it’s a split-night study. Home tests are cheaper - $150 to $500 - but they’re not always accepted for insurance claims if your case is complex.Is There Anything New in Sleep Testing?
Yes. Modern sleep labs are using wireless sensors that cut the number of wires from 20+ down to 5 or 6. Some systems now use AI to help flag abnormal patterns faster. And researchers are testing simplified home polysomnography devices - but so far, nothing matches the accuracy of a lab test. The American Academy of Sleep Medicine says polysomnography will remain the gold standard through at least 2030. Why? Because sleep isn’t just about breathing. It’s about your brain, your heart, your muscles - all working together. And only a full polysomnography can see the whole picture.Common Questions About Sleep Studies
Will I be able to sleep with all those wires on me?
Most people do. While it feels strange at first, the sensors are lightweight and non-invasive. Sleep technologists are trained to help you relax, and many patients report sleeping better than they expected. You don’t need a perfect night - just enough sleep to capture your normal sleep cycles.
Can a polysomnography test miss sleep apnea?
It’s rare, but possible. If your apnea only happens when you sleep on your back and you don’t spend much time in that position during the test, it might not show up. That’s why doctors sometimes recommend a second test or ask you to sleep in a specific position. The test is designed to catch the most common patterns, but not every single event.
Is polysomnography only for sleep apnea?
No. While it’s best known for diagnosing sleep apnea, it’s also the only test that can confirm narcolepsy, restless legs syndrome, night terrors, sleepwalking, and even nocturnal seizures. If you have unusual nighttime behaviors or extreme daytime fatigue without obvious cause, a full polysomnography is essential.
What if I can’t sleep during the test?
You don’t have to sleep like you do at home. As long as you get 4-6 hours of sleep with at least one full sleep cycle (including REM), the data is usable. Technologists can adjust sensors, turn down lights, or even let you get up briefly if needed. The goal is to capture your typical sleep patterns, not perfection.
Can I use my phone or watch TV before bed?
Yes, most sleep centers allow you to watch TV or read until lights out. But avoid screens right before bed - the blue light can delay sleep. The center will usually have a TV in the room, and you can bring your own books or tablet (with screen dimmed).
How long until I get my results?
It usually takes 1 to 2 weeks. The data is complex - over 1,000 pages of recordings - and must be reviewed by a board-certified sleep specialist. Don’t call the clinic after just a few days. Your doctor will schedule a follow-up to explain everything.
Is there a risk of getting sick or injured during the test?
No. Polysomnography is non-invasive and carries no physical risk. The sensors only record your body’s natural signals - they don’t send any electricity or radiation. The only discomfort might be from the adhesive on your skin, which is removed gently the next morning.

gary ysturiz
January 13, 2026 AT 10:37Just had my first sleep study last month and honestly? It was way less scary than I thought. The techs were super chill, and I ended up sleeping better than I have in years. Didn’t even notice the wires after the first 10 minutes. If you’re nervous, just remember: you’re not being judged, you’re being helped.
Jessica Bnouzalim
January 14, 2026 AT 15:14OMG, YES!! I was convinced I’d be awake all night with all those sensors… but I actually slept like a baby!! And the best part? They caught my mild sleep apnea and hooked me up with a CPAP the same night-no second trip!! Life-changing. Seriously, if you’re even a little suspicious about your sleep, just DO IT.
Lelia Battle
January 15, 2026 AT 14:29The elegance of polysomnography lies not merely in its technical comprehensiveness, but in its quiet affirmation that sleep is not a passive state-it is a complex, dynamic physiological symphony. To reduce it to mere breathing metrics is to ignore the orchestra. The EEG, EOG, EMG-they are not wires, they are translators of the subconscious. We owe it to ourselves to listen.
Rinky Tandon
January 16, 2026 AT 01:19Let me tell you something-most people don’t realize that 78% of sleep apnea cases in India are missed because of Western-centric diagnostic criteria. Your AHI thresholds? Built for white, overweight men. I’ve seen women with severe OSA flagged as ‘normal’ because their oxygen dips are ‘too brief.’ You need culturally calibrated norms. This isn’t science-it’s colonial medicine in a lab coat.
Konika Choudhury
January 16, 2026 AT 20:56Why are we spending thousands on fancy machines when Ayurveda has been curing sleep disorders for 5000 years? Just drink warm milk with ashwagandha before bed and sleep on your left side. No wires needed. This whole thing is just Big Sleep trying to sell you a machine.
Darryl Perry
January 16, 2026 AT 21:25The article is overly verbose. 90% of this is fluff. The core facts: 22 sensors, 4-6 hours of sleep needed, AHI >5 = apnea, CPAP fixes it. Everything else is marketing. Stop padding with anecdotes.
Jose Mecanico
January 17, 2026 AT 06:43My wife had the study last year. She was terrified but ended up sleeping better than she has in a decade. The tech even let her bring her own pillow. Small things matter. Just go in with an open mind.
Alex Fortwengler
January 18, 2026 AT 09:01They’re lying to you. The whole sleep study thing? It’s a scam to sell CPAP machines. I did my own research-sleep apnea is mostly caused by toxins in your mattress. I switched to organic cotton and bamboo and my snoring stopped. No wires. No machines. Just truth.
jordan shiyangeni
January 19, 2026 AT 13:45I’ve been studying sleep science for over 20 years and I can tell you this: most people who get polysomnography are just lazy. They don’t want to fix their sleep hygiene. They want a magic box to tell them it’s not their fault. You don’t need a $3,000 machine to know that scrolling until 2 a.m. and drinking espresso at 7 p.m. is why you’re tired. Stop outsourcing your responsibility to a lab.
Abner San Diego
January 19, 2026 AT 23:53Why does it cost so much? Because the system’s rigged. I work in healthcare admin. The labs get paid per study, not per outcome. So they encourage more tests. Home tests are cheaper and 80% as accurate for simple cases. But the insurance companies? They won’t cover home tests unless you jump through 17 hoops. This isn’t medicine-it’s a revenue stream.
Eileen Reilly
January 21, 2026 AT 11:38So I did the study and they said I had RBD… turns out I was just acting out my dreams about fighting zombies. Which is kinda cool? I mean, I’ve always wanted to be a ninja. But now my husband won’t let me sleep in the same bed. Also, the wires itched. And the TV was playing a rerun of The Office. Not the best vibe. Anyway, CPAP is weird but I’m not dying anymore so… yay?