When a drug’s patent runs out, it doesn’t just disappear from the market-it transforms. Suddenly, cheaper versions appear. Prices drop. Prescriptions change. For patients, this can mean lower costs-or confusion. For healthcare systems, it’s a chance to save millions-or a risk of disruption. The key? Planning. And it has to start long before the patent expires.
What Happens When a Patent Expires?
Every new drug starts with a patent that gives the maker exclusive rights to sell it. That usually lasts 20 years from the date it’s filed. But because it takes 7-10 years just to test and get FDA approval, most drugs only have 7-10 years of real market control. Once that clock runs out, other companies can legally make and sell generic versions. Generic drugs aren’t knockoffs. They’re exact copies in active ingredients, dosage, and how they work. The FDA requires them to be bioequivalent-meaning they deliver the same amount of medicine into your bloodstream as the brand name, within a range of 80% to 125%. That’s why they’re safe. And why they cost 80-85% less. But here’s the catch: not all drugs become cheap right away. Some face delays. Some never get cheaper at all.The Patent Cliff 2.0: A $90 Billion Problem
Between 2025 and 2029, over $90 billion in drug sales will lose patent protection. That’s not a number-it’s a tidal wave. Drugs for autoimmune diseases, cancer, and mental health are hitting their expiry dates all at once. Think Humira, Enbrel, and key diabetes medications. These aren’t obscure pills-they’re the backbone of millions of treatment plans. For systems like hospitals and insurers, this is a golden opportunity. A single drug like Humira, which costs over $2,000 a month as a brand, can drop to under $500 with generics. But that only happens if someone plans for it.Why Patients Get Caught Off Guard
Many patients don’t know their drug is about to lose patent protection. They’re told, “We’re switching you to a generic.” No explanation. No warning. Then they get a new pill-different shape, color, or even inactive ingredients-and suddenly feel off. Maybe their stomach acts up. Or their pain doesn’t improve. Or they get a rash. That’s not the generic’s fault. It’s the system’s. Bioequivalence doesn’t mean identical experience. Different fillers, coatings, or release mechanisms can affect how a drug feels in your body. A 2022 Kaiser Family Foundation survey found 37% of patients reported side effects after switching to generics-even though the FDA says they’re equivalent. Patients on chronic meds-like those for hypertension, depression, or rheumatoid arthritis-are especially vulnerable. A sudden switch without counseling can lead to missed doses, confusion, or worse: treatment failure.How Healthcare Systems Should Prepare
Successful systems don’t wait for the patent to expire. They start two years out. Here’s what they do:- Track every patent. In the U.S., over 1,400 drug patents expire each year. Systems that use software like Symphony Health’s PatentSight stay ahead. Those that don’t get blindsided.
- Build a team. Pharmacy, finance, legal, and clinical staff meet regularly. They don’t wait for the CFO to panic.
- Review formularies. Is your current drug still the best choice? Are there multiple generics coming? Which one offers the best price and reliability?
- Test supply chains. When generics flood the market, shortages happen. Suppliers scramble. The first 3-6 months after expiry are the riskiest. Systems that pre-order or lock in contracts avoid disruptions.
- Update clinical guidelines. Doctors need clear rules on when and how to switch patients. One study showed that when clinics had written substitution protocols, patient discontinuation dropped by 35%.
- Train staff and educate patients. Pharmacies should have handouts. Clinics should have talking points. Patients deserve to know: “Your drug is going generic. Here’s why it’s safe. Here’s what to watch for.”
Biosimilars Are Different
Not all drugs are the same. Small-molecule drugs (like statins or antibiotics) are easy to copy. But biologics-drugs made from living cells, like insulin or monoclonal antibodies-are far more complex. They’re not “generics.” They’re “biosimilars.” And they’re harder to make. That means fewer companies can produce them. And that means slower price drops. While small-molecule generics hit 90% market share within a year, biosimilars only reach 38% in two years. Why? Manufacturing is expensive. Regulatory hurdles are high. And some doctors still hesitate to switch. Oncology biosimilars are leading the way-45% adoption within a year. But for autoimmune drugs? Only 18%. That’s a missed opportunity for savings.The U.S. vs. The Rest of the World
In Europe, when a drug loses patent protection, prices drop fast-often to 30-40% of the original cost. Why? Because governments set reference prices. If a brand-name drug costs $100 and the generic is $20, the government pays $20. No negotiation. No rebates. In the U.S., it’s messy. Rebates, formulary tiers, and pharmacy benefit managers (PBMs) create hidden pricing layers. A drug might list for $1,000, but after rebates, the net price is $600. Then a generic comes in at $150-but the PBM gets a rebate from the brand, so they don’t push the cheaper option. Result? U.S. prices fall slower. Savings take longer. And patients pay more out-of-pocket.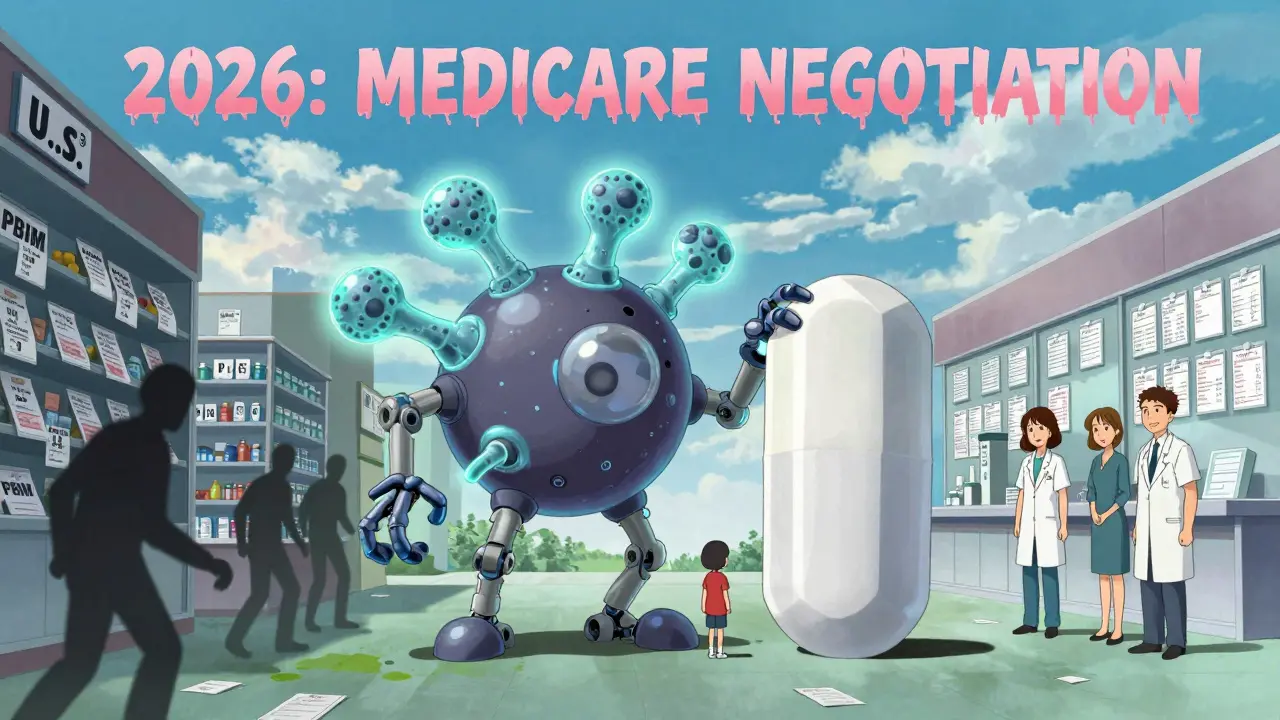
What Patients Can Do Right Now
You don’t need a team. But you do need to be informed.- Check your drug. Use the FDA’s Orange Book or ask your pharmacist: “Is my drug about to lose patent protection?”
- Ask about alternatives. If your drug is expiring soon, ask: “Are there cheaper generics or biosimilars available? Which one do you recommend?”
- Don’t assume the new pill is the same. If you feel different after switching, tell your doctor. It’s not “all in your head.”
- Ask for transition support. Many pharmacies now offer free counseling when switching to generics. Use it.
- Monitor your bills. Sometimes, the switch doesn’t save you money because your insurance plan still favors the brand. Ask your insurer: “Will my copay drop when the generic comes?”
What’s Changing in 2026 and Beyond
The Inflation Reduction Act of 2022 started Medicare drug price negotiations. Starting in 2026, Medicare will negotiate prices for 10-20 high-cost drugs that just lost patent protection. That’s a game-changer. It forces manufacturers to lower prices-or lose Medicare sales. New laws like the CREATES Act are also cracking down on “pay-for-delay” deals-where brand companies pay generics to stay off the market. The FTC says these deals dropped 35% in 2023. And AI is helping. Health systems using AI to predict patent expirations now forecast with 89% accuracy-up from 65%. That means fewer surprises.The Bottom Line
Patent expiry isn’t a crisis. It’s a transition. And transitions are easier when you plan. For patients: Know your drug. Ask questions. Speak up if something feels off. For systems: Start two years out. Track patents. Train staff. Educate patients. Lock in contracts. Don’t wait for the price to drop-make it drop. The savings are real. Billions of dollars. Better access. Lower out-of-pocket costs. But only if we act before the patent expires-not after.What happens to drug prices after patent expiry?
After a drug’s patent expires, generic versions enter the market. Prices typically drop by 80-85% within the first year for small-molecule drugs. For biosimilars, the drop is slower-usually 20-40% in the first year-because they’re harder to manufacture. In the U.S., prices decline gradually due to rebates and formulary deals, while in Europe, they often drop faster because of government price controls.
Why do some patients feel different after switching to a generic drug?
Even though generics must be bioequivalent to the brand-name drug, they can contain different inactive ingredients-like fillers, dyes, or coatings. These can affect how the drug is absorbed or how it feels in your body. Some patients report stomach upset, dizziness, or reduced effectiveness after switching. It’s rare, but it happens. If you notice changes, talk to your doctor. You may need to try a different generic version.
How long before patent expiry should healthcare systems start planning?
The most successful systems begin planning at least 24 months before the patent expires. This gives them time to track upcoming generics, negotiate contracts, update formularies, train staff, and educate patients. Systems that wait until 12 months out save 22% less on average, according to the Healthcare Financial Management Association.
Are biosimilars the same as generics?
No. Generics are exact chemical copies of small-molecule drugs. Biosimilars are highly similar versions of complex biologic drugs made from living cells. They’re not identical because their manufacturing process is too intricate to replicate perfectly. That’s why biosimilars take longer to develop, cost more, and enter the market slower than generics. But they still offer major cost savings.
Can patent expiry be delayed?
Yes. Drugmakers often use tactics like “patent thickets”-filing dozens of secondary patents on minor changes like dosage forms, delivery methods, or packaging-to delay generic entry. These can extend exclusivity by years. The FDA and FTC are cracking down, but it still happens. Systems that use patent-tracking software can anticipate these delays and adjust their plans accordingly.
What role does Medicare play in patent expiry now?
Starting in 2026, Medicare will negotiate prices for up to 20 high-cost drugs that have lost patent protection. This is part of the Inflation Reduction Act. It forces manufacturers to lower prices or lose Medicare sales. This is expected to drive down costs faster than market forces alone, especially for drugs used by seniors.

Suzette Smith
February 10, 2026 AT 20:00Okay but have you ever tried switching to a generic and then your anxiety went from manageable to ‘I need to call a therapist and also a lawyer’? I’m not saying generics are bad-I’m saying the system is lazy. They swap you out like you’re a lightbulb and expect you to just ‘adapt.’ No one asks if you slept. No one asks if your knees still work. Just ‘here’s a blue pill now.’ Thanks, America.
Sophia Nelson
February 12, 2026 AT 00:46Let’s be real-the entire pharmaceutical industry is a pyramid scheme. Patent expiry? More like ‘patent delay with a side of bribery.’ Big Pharma pays off politicians, PBMs, and even some doctors to keep prices high. The FDA? A revolving door. And now they want us to trust generics? Please. I’ve seen the same generic made in three different countries with three different side effect profiles. This isn’t healthcare. It’s a casino.
Reggie McIntyre
February 13, 2026 AT 05:31Man, I love how this article doesn’t just throw numbers at us-it actually *humanizes* the transition. I work in a rural clinic, and last year we switched 47 patients off a brand-name biologic to a biosimilar. We did it slow. We had one-on-one chats. We gave out color-coded charts. We even had a pharmacist do a live Q&A over Zoom. And guess what? Only two patients dropped out. The rest? They saved $1,200 a month. That’s a mortgage payment. That’s groceries. That’s not just cost-cutting-that’s dignity. We didn’t just change pills. We changed lives.
Carla McKinney
February 14, 2026 AT 07:33Let’s dissect this. The article says ‘start planning two years out.’ But that’s only true if you’re a hospital with a $20M pharmacy budget. Most community clinics? They’re lucky if they get a spreadsheet update. And ‘training staff’? Who? The nurse who’s already working 60 hours a week? The ‘formulary review’ process? It’s a PowerPoint deck buried under 17 other priorities. This isn’t guidance-it’s a fantasy written by someone who’s never seen a Medicaid patient’s prescription log.
Ojus Save
February 15, 2026 AT 19:18yea i read this and i was like wow but what about in india? we get generics for like 10 dollars a month and no one even talks about it. its just… there. no drama. no switching. no confusion. just a little pill in a plain box. maybe the problem is not the generic. maybe its the overthinking.
Jack Havard
February 17, 2026 AT 01:26Patent expiry is just the tip of the iceberg. What they don’t tell you is that the FDA’s bioequivalence standards are based on healthy volunteers-not people with liver disease, kidney failure, or autoimmune disorders. So when they say ‘80-125% bioequivalence,’ what they really mean is ‘it works for someone who doesn’t have a chronic illness.’ For the rest of us? It’s a crapshoot. And the system knows it. They just don’t care enough to fix it.
Jonathan Noe
February 17, 2026 AT 21:14Here’s the thing no one’s talking about: the real bottleneck isn’t the generic manufacturers-it’s the pharmacy benefit managers. They control formularies. They get kickbacks from brand-name drugs. And they actively discourage switches because the rebate structure is more profitable for them. If you want real change, don’t focus on the patent clock. Focus on dismantling the PBM monopoly. That’s where the money’s hiding. And that’s where the real fight needs to be.
Autumn Frankart
February 18, 2026 AT 18:53Mark my words-this is all part of a globalist agenda to weaken American healthcare sovereignty. The same people pushing generics are the ones who want to import drugs from China and India. And do you know what’s in those pills? No one’s tested them. No one’s auditing them. We’re letting foreign labs make our life-saving meds while our own labs sit idle. This isn’t savings. This is surrender. And soon, you’ll see the side effects… and they won’t be from the pills. They’ll be from the fear.
Stephon Devereux
February 19, 2026 AT 10:04Patent expiry isn’t about cost-it’s about continuity. It’s about the quiet dignity of being able to take your medicine without being treated like a data point. The real innovation here isn’t in chemistry-it’s in compassion. When we design systems that treat patients as humans-not line items-we don’t just save money. We save trust. And trust? That’s the one thing no algorithm can replicate. Start with empathy. The rest will follow.
Neha Motiwala
February 19, 2026 AT 22:40Okay, but what about the people who get rashes? Or seizures? Or panic attacks? I know someone who switched to a generic and had to be rushed to the ER because her heart started fluttering. They said it was ‘coincidental.’ But she’d been stable for 8 years. Coincidence? No. It was the pill. And now? She’s off all meds. And she’s not alone. They’re not telling you this because they don’t want you to panic. But you should. Because they’re not testing on us. They’re testing on our bodies. And we’re the lab rats.