When a patient picks up a generic pill, they don’t just see a cheaper version of their branded medicine. They see a color, a shape, a size-and sometimes, a hidden ingredient that goes against their beliefs. For many people around the world, the difference between a branded pill and its generic copy isn’t just about cost. It’s about trust, religion, culture, and even identity.
Why a Generic Pill Feels Wrong to Some Patients
In the U.S., nearly 9 out of 10 prescriptions are filled with generic drugs. They’re safe, effective, and save billions every year. But for some patients, especially those from Black, Hispanic, Muslim, or Jewish communities, taking a generic can feel like a betrayal. Why? Because generics often look nothing like the brand-name version they’re used to. A 2022 FDA survey found that 28% of African American patients believed generic medications were less effective than branded ones. Among non-Hispanic White patients, that number was just 15%. The gap isn’t about science-it’s about perception. In many cultures, the appearance of a pill matters. A red capsule might mean strength. A white tablet might feel like water. A pill that’s too small or oddly shaped can trigger doubts: Is this really the same medicine? One pharmacist in Chicago told a story about a Somali patient who refused a generic metformin because it was a yellow capsule. The patient had taken the same branded version for years-bright blue. To them, yellow meant something weaker, maybe even unsafe. The pharmacist spent two hours calling manufacturers until they found a generic version in blue. The patient filled the prescription the next day.Hidden Ingredients That Break Religious Rules
Generic drugs are made with the same active ingredient as the brand name, but the fillers-called excipients-can be wildly different. Gelatin, lactose, dyes, and preservatives are often swapped out to cut costs. For most people, that’s fine. For others, it’s a dealbreaker. Muslim patients may refuse medications containing pork-derived gelatin, which is common in capsules. Jewish patients may avoid products not certified kosher. Hindu patients might object to bovine gelatin. In one 2023 study, 63% of pharmacists in urban areas said they received at least one question per week about whether a medication contained forbidden ingredients. The problem? Most generic drug labels don’t say. Only 37% of generic medication inserts in the U.S. list excipients in detail. In the EU, where regulations are stricter, that number is 68%. That means patients and pharmacists are often left guessing-or worse, assuming. A Muslim woman with diabetes once stopped her generic insulin because she found out the capsule shell contained pork gelatin. She didn’t tell her doctor. She just stopped taking it. Her blood sugar soared. She didn’t want to be judged. She didn’t want to cause trouble. She just wanted to follow her faith-and stay healthy.Language, Color, and the Power of Perception
It’s not just about what’s inside the pill. It’s about how it’s presented. In some Latin American cultures, blue pills are associated with healing. In parts of Asia, green means natural and safe. In Western cultures, white often signals purity. Change the color, and you change the meaning. One study showed that patients from India were more likely to trust a generic pill if it was round and white-just like the branded version they remembered. A green oval? They’d think it was a different drug. Language barriers make it worse. A Spanish-speaking patient might get a pill bottle with instructions printed only in English. A Vietnamese grandmother might not understand what “take once daily” means if the label doesn’t say “mỗi ngày một lần.” And let’s not forget the stigma. Some patients believe generics are “leftover” drugs-cheap, low-quality, or even experimental. That belief doesn’t come from nowhere. It’s shaped by years of unequal care, mistrust in the system, and stories passed down in families: “The hospital gave me the cheap pills. My cousin got sick after taking them.”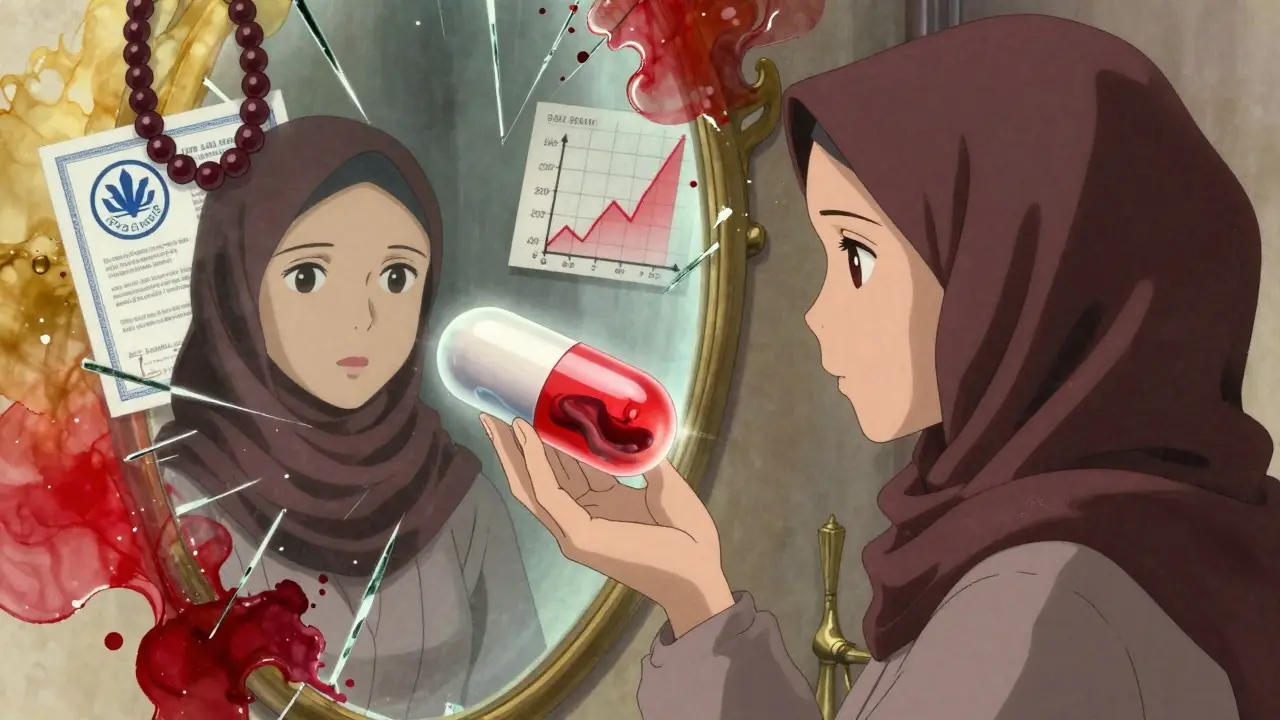
What Pharmacies Are Doing Right
Some pharmacies are stepping up-not because they’re forced to, but because they see the need. One chain in New Jersey created a digital database that flags every generic medication for halal, kosher, vegan, and color-sensitive options. Staff get 10 hours of training each year on cultural competence. They keep a list of alternative formulations on hand. If a patient asks for a gelatin-free version of their generic levothyroxine, they can pull up a match in under a minute. Teva Pharmaceutical launched a “Cultural Formulation Initiative” in 2023. By the end of 2024, they plan to document excipient details for all 15 major therapeutic areas-something no other generic maker has done at this scale. Sandoz announced a similar global framework in early 2024. These aren’t just nice gestures. They’re smart business. The U.S. market alone has an estimated $12.4 billion in unmet need among minority populations-mostly because people aren’t taking their meds. Hypertension and diabetes treatments are the biggest gaps. Fix the cultural barriers, and you fix adherence.The Gap Between Policy and Practice
The Food and Drug Omnibus Reform Act (FDORA) passed in December 2022 pushed for better inclusion in clinical trials and more attention to social determinants of health. That’s a big step. But laws don’t change pill colors or ingredient lists. Only 22% of community pharmacies in the U.S. have formal training on cultural considerations for generics. Most pharmacists learn on the job-by trial and error. Many don’t know how to ask the right questions. Others fear offending patients by bringing up religion or culture. And manufacturers? Most still treat cultural needs as an afterthought. Generic drugs are designed for volume, not personalization. If a formulation works for 80% of people, they move on. The other 20%? They’re told to adapt. But patients shouldn’t have to choose between their faith and their health.
What Patients Can Do
If you’re taking a generic and you’re unsure about the ingredients:- Ask your pharmacist: “Does this contain gelatin, lactose, or animal products?”
- Request the full ingredient list. You have the right to know.
- If the pill looks different, ask if there’s another version available that matches your old one.
- Don’t stop taking your medication without talking to someone. There’s almost always a solution.
What Providers and Pharmacies Can Do
Pharmacists are on the front lines. They need tools, not just good intentions.- Create a simple checklist: Does this medication contain gelatin? Is it kosher? Is the color culturally acceptable?
- Keep a list of alternative generics with approved excipients.
- Train staff on how to ask culturally sensitive questions without making assumptions.
- Partner with local religious leaders to understand community needs.
- Use multilingual, visual pill guides-images of pills with names in multiple languages.
The Future of Generics Is Inclusive
By 2027, 65% of top generic manufacturers plan to include cultural considerations in their product design. That’s up from just 15% in 2023. It’s happening-not because it’s trendy, but because it’s necessary. Generics are meant to make medicine accessible. But access isn’t just about price. It’s about respect. It’s about honoring someone’s beliefs while keeping them healthy. The science of generics is solid. The problem isn’t the medicine. It’s the system that ignores the people who take it. Change starts with a simple question: Does this pill work for you? Not just medically-but culturally, spiritually, and personally. If we want real health equity, we have to stop treating culture as an add-on. It’s part of the prescription.Why do some patients refuse generic medications?
Patients may refuse generics because the pills look different from the branded version they’re used to-different color, shape, or size. In some cultures, these visual changes signal lower quality or even danger. Others refuse because the medication contains ingredients like pork gelatin or alcohol, which conflict with religious beliefs. Misinformation, past experiences with poor care, and language barriers also contribute to distrust.
Are generic medications less effective than brand-name drugs?
No. By law, generic medications must contain the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also meet the same FDA standards for safety and effectiveness. The only differences are in inactive ingredients (excipients) and appearance. Studies consistently show generics work just as well. But if a patient believes they’re less effective, their adherence drops-and that affects outcomes.
What are excipients, and why do they matter in multicultural care?
Excipients are inactive ingredients in medications-like fillers, dyes, and capsule shells. They don’t treat the condition, but they can cause real problems. For example, pork gelatin in capsules violates halal dietary laws for Muslims. Lactose can be an issue for some Jewish communities or those with cultural aversions. Color dyes may carry symbolic meanings in certain cultures. These ingredients are often not clearly listed on U.S. generic labels, making it hard for patients to make informed choices.
How can pharmacists better support patients from diverse backgrounds?
Pharmacists can start by asking open-ended questions: “Is there anything about this medication that might not work for you?” They should keep a list of culturally appropriate alternatives, train staff on religious and cultural norms, and use multilingual visual aids. Some pharmacies now use digital tools to quickly check if a generic contains gelatin, alcohol, or other restricted ingredients. Building trust means listening more than explaining.
Is there a difference in how generics are regulated in the U.S. versus Europe?
Yes. In the European Union, regulations require more detailed labeling of excipients on generic medications-68% of EU labels include full ingredient lists, compared to only 37% in the U.S. The EU also has stricter rules on allergen disclosure and religious considerations. This gives European pharmacists and patients more information to make culturally informed choices. The U.S. is slowly catching up, but progress has been uneven.
What’s being done to improve cultural competence in the generic drug industry?
Major manufacturers like Teva and Sandoz have launched initiatives to document and standardize excipient information across their generic products. Teva’s Cultural Formulation Initiative aims to fully map ingredients for 15 major drug categories by late 2024. Sandoz is developing a global framework to ensure cultural compatibility in packaging and labeling. Some pharmacy chains now offer halal- and kosher-certified generic options. These efforts are still limited, but they’re growing fast as companies realize cultural competence improves adherence and market reach.

Tru Vista
January 1, 2026 AT 21:20Generic = lazy pharma. Same active ingredient? Sure. But excipients? Totally different. And no one tells you. That’s not transparency, that’s corporate negligence. 🤡
Philip Leth
January 3, 2026 AT 02:12My cousin’s a pharmacist in Philly. He told me a Somali guy refused a generic because it was yellow. So he spent 3 hours tracking down a blue version. The guy cried. That’s not science-that’s human. We treat meds like widgets. We’re wrong.
Neela Sharma
January 3, 2026 AT 04:44In India, we know pills by color. White = safe. Green = natural. Red = strong. If your generic looks like a toy, we don’t trust it. No label in Hindi? Even worse. You think science fixes this? No. Respect does.
Tiffany Channell
January 4, 2026 AT 01:07Oh please. People refuse generics because they’re lazy and paranoid. The science is solid. If you don’t trust your doctor, that’s your problem, not the FDA’s. Stop romanticizing ignorance.
JUNE OHM
January 4, 2026 AT 09:23They’re letting Muslims dictate pill colors now? 😂 Next they’ll ban red dye because it’s ‘too aggressive’ for the Chinese. This isn’t medicine, it’s woke branding. The FDA should stop caving to cultural tantrums. 💩
Angela Fisher
January 6, 2026 AT 00:01They don’t tell you this but the same factories make branded and generic pills. Same machines. Same workers. Just different labels. The brand name costs $12. The generic? $1.20. Who’s really being ripped off? The system. The corporations. The whole damn thing. 🕵️♀️
And don’t get me started on gelatin. You think pork gelatin is the only thing hiding in your meds? What about the dyes? The preservatives? The ones that come from animal bones? They don’t list those. They don’t have to. You’re being fed lies every time you swallow a pill.
My grandma took a generic for her heart and got sick. She didn’t know the capsule had gelatin from pigs. She was Muslim. She didn’t say anything. She just stopped. Died three months later. No one asked. No one cared. Now they want to ‘train pharmacists’? Too late.
They’ll never fix this. Because fixing it means admitting the system is broken. And nobody wants to admit that. Not the pharma giants. Not the politicians. Not even the pharmacists who know the truth.
They call it ‘adherence.’ I call it silent suffering. People don’t take their meds because they’re scared. Not because they’re stupid. Because they’ve been lied to for decades. And now they’re just trying to survive.
And now they want to slap a ‘halal certified’ sticker on it like that fixes everything? No. It’s a band-aid on a hemorrhage. The real problem? Profit over people. Always has been. Always will be.
So yeah. Color matters. Gelatin matters. Language matters. But none of it matters if the system doesn’t change. And it won’t. Because change costs money. And money talks louder than faith.
Angela Goree
January 7, 2026 AT 08:18Who gave them the right to demand blue capsules?! This is America! We don’t cater to cultural whims! If you can’t trust science, then don’t take the pill! End of story!!!
Joy F
January 9, 2026 AT 06:19It’s not about gelatin. It’s about epistemic violence. The pharmaceutical-industrial complex weaponizes biosemiotics to erase cultural epistemologies. The pill is a colonial artifact-its color, its shape, its inert matrix-all engineered to assimilate the body into a neoliberal pharmacopeia. You think this is about medicine? No. It’s about control. And the silence? That’s the real toxicity.
Lori Jackson
January 10, 2026 AT 19:41Wow. So now we’re supposed to redesign every generic drug because some people are ‘sensitive’? This is what happens when you let emotion override science. Next thing you know, we’ll need kosher aspirin and vegan ibuprofen. It’s absurd. And expensive. And frankly, infantilizing.
Michael Burgess
January 12, 2026 AT 17:55My aunt in Detroit stopped her blood pressure meds because the generic looked like a candy. She said it felt like the hospital was messing with her. I didn’t know what to say. So I took her to the pharmacy. We asked for the blue version. They had it. She cried. We all did. It’s not about science. It’s about dignity. And yeah, it’s that simple.
Shruti Badhwar
January 14, 2026 AT 01:05India has over 1.3 billion people. We’ve been using generics for decades. We don’t need a ‘cultural formulation initiative.’ We need better labeling. And yes, we know the difference between a yellow and blue capsule. It’s not superstition. It’s experience. Give us the facts. We’ll make the choice.
Haley Parizo
January 15, 2026 AT 06:34Let me be clear: culture isn’t a ‘feature’ to be optimized. It’s the foundation of how people experience health. To treat it as a marketing afterthought is not just unethical-it’s deadly. If a woman stops her insulin because the capsule shell is made from pig fat, that’s not a ‘compliance issue.’ That’s a moral failure of the entire healthcare system. We don’t need more training. We need accountability.
Ian Detrick
January 17, 2026 AT 04:35Here’s the truth: generics saved my life. But I also know people who died because they didn’t trust them. The solution isn’t to shame them. It’s to listen. Ask. Adapt. The science is solid. But the system? It’s broken. And fixing it starts with a question: ‘Does this pill work for you?’ Not just in your blood. In your soul.