Every year, thousands of seniors end up in the hospital-not because of a fall, heart attack, or infection, but because of a medication they were told was safe. It’s not always the dose. It’s often the drug itself.
Why Some Medications Are Dangerous for Seniors
As we age, our bodies change. The liver slows down. Kidneys don’t filter as well. Brain chemistry shifts. What was a harmless pill at 50 can become a danger at 75. That’s why doctors use the Beers Criteria-a list updated every two years by the American Geriatrics Society-to flag medications that are riskier than they’re worth for people over 65. These aren’t just "maybe" risks. These are proven dangers. A 2023 study found that 36% of older adults in the U.S. are taking at least one medication on this high-risk list. And nearly half of seniors take five or more prescriptions. That’s called polypharmacy-and it multiplies the risk of bad reactions, falls, confusion, and even death.Top 5 High-Risk Medications for Seniors
Not all drugs are created equal when it comes to aging bodies. Here are five that should be reviewed right away:- Zolpidem (Ambien®) - This sleep aid doesn’t just help you fall asleep. It can make you sleepwalk, fall, or wake up confused the next morning. For seniors, it increases fall risk by 82% and doubles the chance of hip fractures. The effects can last over 11 hours-even after you think you’ve "slept it off."
- Glyburide (Diabeta®) - Used for type 2 diabetes, this older drug causes dangerous low blood sugar in nearly 30% of seniors. Compared to newer options like glipizide, it’s over twice as likely to send someone to the ER. The FDA now requires a boxed warning on its label for patients over 65.
- Diphenhydramine (Benadryl®) - Found in sleep aids, allergy pills, and even some cold medicines, this antihistamine has a high anticholinergic score. Long-term use raises dementia risk by 54%. It also causes dry mouth, constipation, and urinary retention-all common and painful problems in older adults.
- Promethazine (Phenergan®) - Often given for nausea or vomiting, this drug can cause severe drowsiness, tremors, and even seizures in seniors with Parkinson’s or epilepsy. Many families report relatives becoming "zombie-like" for 24 hours after one dose.
- Alpha-1 blockers (Doxazosin, Terazosin) - Prescribed for prostate issues or high blood pressure, these drugs drop blood pressure too fast when standing. One in four seniors on these medications gets dizzy or faints. That’s 3 times higher than with safer alternatives like chlorthalidone.
What Makes These Drugs So Risky?
It’s not just about the drug. It’s about how aging bodies handle it. Older kidneys can’t clear drugs like they used to. That means medications build up in the system. Liver enzymes slow down, so drugs stay active longer. The brain becomes more sensitive to sedatives. And when you’re taking five pills, one can react with another in ways doctors don’t always predict. For example, mixing ciprofloxacin (an antibiotic) with warfarin (a blood thinner) can spike INR levels by 47%. That means a higher chance of internal bleeding. Or taking nitrofurantoin (for UTIs) with poor kidney function? That can cause fatal lung damage in 18% of cases. The Anticholinergic Cognitive Burden (ACB) scale helps measure this. Drugs like amitriptyline (Elavil®) score a 3-meaning they’re high risk. Cumulative use over 1,095 days increases dementia risk by 54%. That’s not a small side effect. That’s a life-altering one.
What Are the Safer Alternatives?
There’s almost always a better option. You don’t have to live with poor sleep, high blood pressure, or diabetes just because the old drug was "good enough."- Instead of zolpidem: Try trazodone (low dose) or cognitive behavioral therapy for insomnia (CBT-I). Studies show CBT-I works better than pills for seniors-and has no risk of falls.
- Instead of glyburide: Use glipizide or metformin. Glipizide clears faster, so it’s less likely to cause low blood sugar overnight.
- Instead of diphenhydramine: Use loratadine (Claritin) or cetirizine (Zyrtec). They don’t cross the blood-brain barrier, so no brain fog.
- Instead of promethazine: Try ondansetron (Zofran) for nausea. It’s just as effective, with no risk of tremors or seizures.
- Instead of alpha-1 blockers: Use chlorthalidone or ACE inhibitors for blood pressure. They’re gentler on balance and blood flow.
How to Get Your Medications Reviewed
You don’t need to wait for a crisis. Start now. Do a "brown bag" review. Take every pill, capsule, and patch you take-including vitamins, supplements, and over-the-counter meds-to your doctor or pharmacist. Ask: "Which of these are on the Beers Criteria list?" Ask about anticholinergic burden. Request the Anticholinergic Risk Scale (ARS) score for your meds. If it’s over 3, you’re at high risk. Check your Medicare plan. Almost all Medicare Advantage plans use the Beers Criteria to limit coverage. If your drug is denied, it’s not random-it’s because it’s known to be dangerous. Bring a pharmacist in. Pharmacists are trained to spot interactions. Studies show pharmacist-led reviews reduce high-risk medication use by 35% in six months. Use electronic alerts. Most major EHR systems (like Epic and Cerner) now flag Beers Criteria drugs at the point of prescribing. Ask your doctor if they’re using these tools.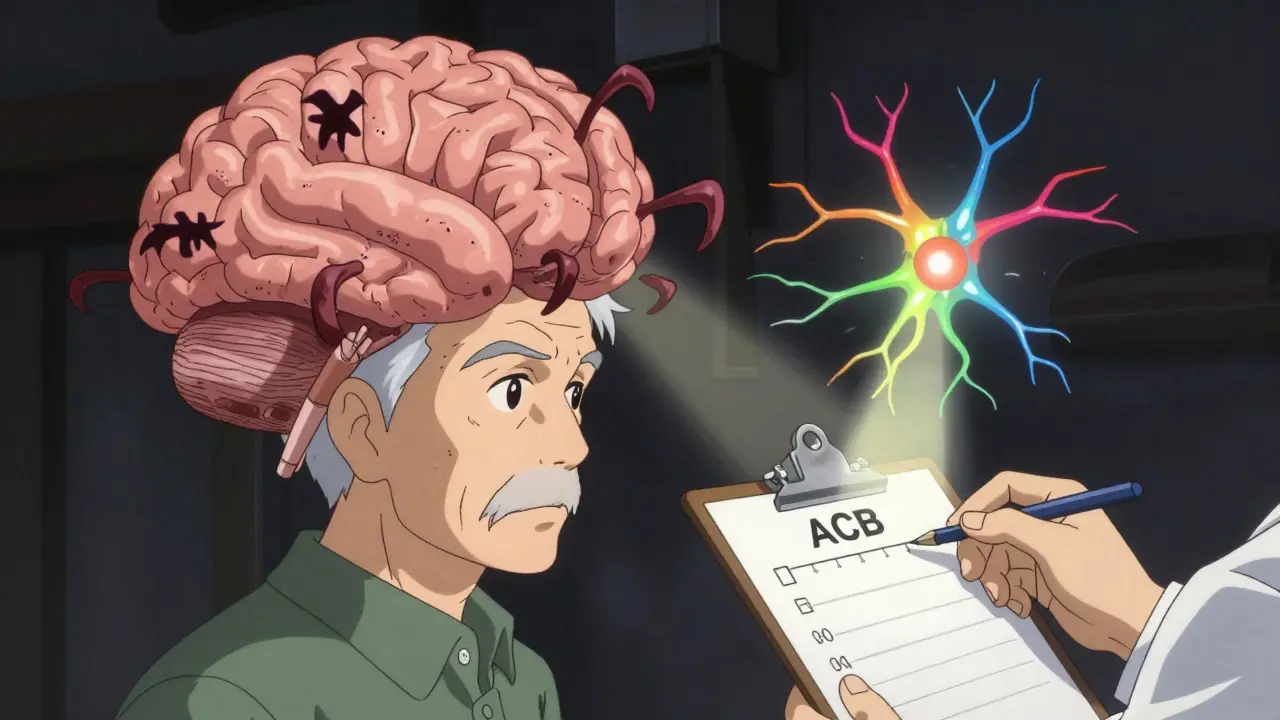
What to Do If You’re Already on One of These Drugs
Don’t stop cold turkey. Some drugs, like benzodiazepines or sleep aids, can cause withdrawal seizures if stopped suddenly. Work with your provider on a taper plan. Most safe transitions take 4 to 6 weeks. For insomnia, combine tapering with CBT-I. For pain, try physical therapy or acetaminophen instead of opioids like meperidine (Demerol®), which can trigger seizures in seniors due to toxic metabolites. One woman in Melbourne, 78, was on amitriptyline for nerve pain. She got constipated, confused, and fell twice. Her doctor switched her to duloxetine. Within two weeks, her pain stayed controlled-and her confusion and falls stopped.Why This Matters More Than Ever
In 2022, adverse drug events cost Medicare $177 billion. That’s money spent on hospital stays, emergency rooms, and long-term care that could have been avoided. And here’s the hard truth: 58% of seniors on high-risk meds didn’t even know there was a safer option. Only 32% had a conversation with their doctor about the risks. This isn’t about being "anti-medication." It’s about being smart with medication. Aging isn’t a disease. But many of the drugs we give to older adults treat aging like it is.Questions to Ask Your Doctor
- Is this drug on the Beers Criteria list?
- What’s the anticholinergic score?
- Is there a safer alternative with fewer side effects?
- Can we try a lower dose or stop it altogether?
- How will we know if it’s working-or causing harm?
Medication safety isn’t a one-time checkup. It’s an ongoing conversation. And for seniors, it might be the most important one they ever have.
What is the Beers Criteria?
The Beers Criteria is a list of medications that are potentially inappropriate for older adults, especially those over 65. Developed by the American Geriatrics Society and updated every two years, it identifies drugs that carry higher risks of side effects like falls, confusion, kidney damage, or death in seniors. It’s used by doctors, pharmacists, and Medicare plans to guide safer prescribing.
Can I just stop taking a high-risk medication?
No. Stopping some medications suddenly can cause serious withdrawal symptoms, seizures, or rebound effects. Always work with your doctor to create a tapering plan. For example, sleep aids like zolpidem or benzodiazepines need to be slowly reduced over weeks, often with support from cognitive behavioral therapy.
Are over-the-counter drugs safe for seniors?
Not always. Many OTC meds like diphenhydramine (Benadryl), ibuprofen, and cold remedies have hidden risks. Diphenhydramine increases dementia risk. Ibuprofen can cause kidney damage or stomach bleeding in older adults. Always check with a pharmacist before taking any non-prescription drug.
How often should seniors have their medications reviewed?
At least once a year, but every 3 to 6 months is better if you’re on five or more medications. If you’ve recently been hospitalized, had a fall, or started a new drug, schedule a review right away. Medicare requires annual medication reviews for beneficiaries in its Medication Therapy Management program.
Do pharmacies know about the Beers Criteria?
Yes. Most U.S. pharmacies use systems like Surescripts that flag Beers Criteria drugs at the point of sale. If you’re prescribed a high-risk medication, your pharmacist may call your doctor to suggest a safer alternative. Always ask your pharmacist to review your full list of meds.
What if my doctor says the drug is necessary?
Ask why. Request the evidence. Is this drug being used for a condition it was designed for? Are there alternatives with better safety profiles? Sometimes, a drug is prescribed out of habit. If you’re uncomfortable, ask for a second opinion or a referral to a geriatric pharmacist.

Paula Villete
December 22, 2025 AT 18:14Okay, but can we talk about how we’re treating aging like it’s a glitch to be fixed with pills? I’m 72 and my grandma took three of these ‘dangerous’ meds for 20 years and still danced at my wedding. Not saying we ignore the risks-but let’s not infantilize older people either. Some of us know our bodies better than the latest Beers Criteria update.
Also, ‘zombie-like’ after promethazine? That’s not a medical term. That’s my uncle after Thanksgiving dinner. Just sayin’.
Georgia Brach
December 24, 2025 AT 08:20The data presented is statistically misleading. The 36% figure includes patients on these medications for documented, clinically necessary indications-many of which have no viable alternatives. To suggest these drugs are universally dangerous ignores individual variability in metabolism, comorbidities, and pharmacogenomics. Furthermore, the Beers Criteria is not evidence-based medicine; it’s a consensus document subject to institutional bias and pharmaceutical lobbying cycles.
Replacing glyburide with glipizide? Glipizide still carries hypoglycemia risk. The real issue is inadequate monitoring protocols, not the drugs themselves. This article is fear-mongering dressed as public health advice.
Lu Jelonek
December 24, 2025 AT 17:48I’ve worked as a geriatric pharmacist for 28 years, and this is one of the clearest summaries I’ve seen. The Beers Criteria isn’t perfect, but it’s the best tool we have to prevent harm. I’ve seen too many seniors on diphenhydramine for sleep-then end up in the ER with urinary retention and delirium. It’s heartbreaking.
And yes, OTC meds are the silent killers. I always tell patients: if it’s in the ‘sleep aid’ aisle, it’s probably not safe for you anymore. Loratadine instead of Benadryl? Easy swap. CBT-I instead of Ambien? Life-changing.
Bring your brown bag. Ask your pharmacist. You deserve to feel clear-headed, not foggy and fragile.
Ademola Madehin
December 25, 2025 AT 05:54YOOOOOOO I JUST REALIZED MY MOM TAKES ALL FIVE OF THESE AND SHE’S BEEN WALKING LIKE A ROBOT SINCE LAST CHRISTMAS 😭
She says ‘it’s just how you get old’ but NO. She was dancing to Beyoncé last year. Now she just stares at the TV and forgets her name. I’m taking her to a geriatric pharmacist TOMORROW. THIS ARTICLE SAVED MY MOM’S LIFE 💔🙏
Diana Alime
December 25, 2025 AT 08:15So… wait. You’re saying my grandpa’s 17 pills are dangerous? But he’s been on them since 2008 and he still argues with me about the Patriots. He’s fine!
Also, CBT-I? Like… therapy for sleep? I can’t even get my cat to sleep on the bed. How’s that gonna work for someone who forgets where they put their glasses?
Also also-why is this on Reddit? Shouldn’t this be a pamphlet at CVS? 🤔
claire davies
December 26, 2025 AT 10:45I’ve spent years watching my mother-in-law navigate this minefield-between Medicare denials, doctors who won’t listen, and pharmacies that don’t flag interactions. What struck me most is how little we’re taught about this as a culture. We’re raised to trust prescriptions like they’re holy writ.
But the truth? Your pharmacist knows more about your meds than your doctor sometimes. I once walked into a pharmacy with my mom’s 14-pill list and the pharmacist said, ‘You’re lucky she’s still standing.’ We cut six meds in six weeks. Her balance improved. Her mood lifted. She started gardening again.
This isn’t about being anti-drug. It’s about being pro-life. Pro-clarity. Pro-dignity. And honestly? Pro-pharmacist. They’re the unsung heroes of aging well.
Raja P
December 26, 2025 AT 20:06Really appreciate this breakdown. I’m from India and we don’t have Beers Criteria here-but my uncle had a similar story with amitriptyline. He was on it for nerve pain, got super constipated, confused, and almost fell down the stairs. We switched to duloxetine and it was night and day.
Also, I never knew diphenhydramine was in so many cold meds. My grandma was taking NyQuil every night. Now we use saline nasal spray and honey tea. Simple. Safe.
Thanks for the actionable advice. This is the kind of info that should be in every senior’s home.
Harsh Khandelwal
December 28, 2025 AT 18:54Wait… so the government and Big Pharma are secretly pushing dangerous drugs on seniors to keep them docile and dependent? And this Beers Criteria thing? A distraction. They don’t want you to know that melatonin and turmeric work better than half these pills.
Also, CBT-I? That’s just a fancy way of saying ‘stop taking pills and think about your trauma.’ My aunt tried it and she cried for three days. Now she’s on a different pill. Coincidence? I think not.
They’re gaslighting us with ‘evidence.’