Most people think of irritable bowel syndrome (IBS) as a belly problem-cramps, bloating, diarrhea, or constipation. But if you’ve lived with it, you know it’s more than that. It’s the anxiety that hits before a meeting. The sleepless nights because your gut won’t quiet down. The frustration of doctors saying "it’s all in your head"-even when the pain is real. The truth is, IBS isn’t just a gut disorder. It’s a breakdown in communication between your gut and your brain. And understanding that connection is the key to real relief.
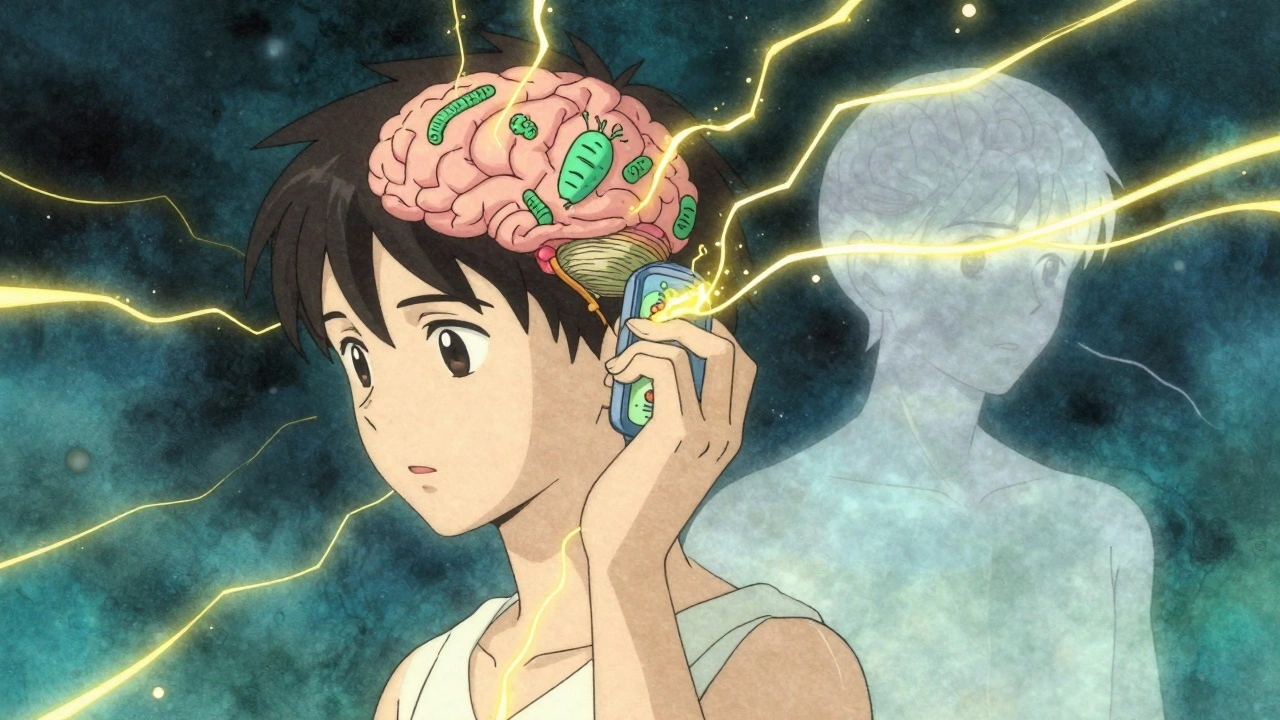
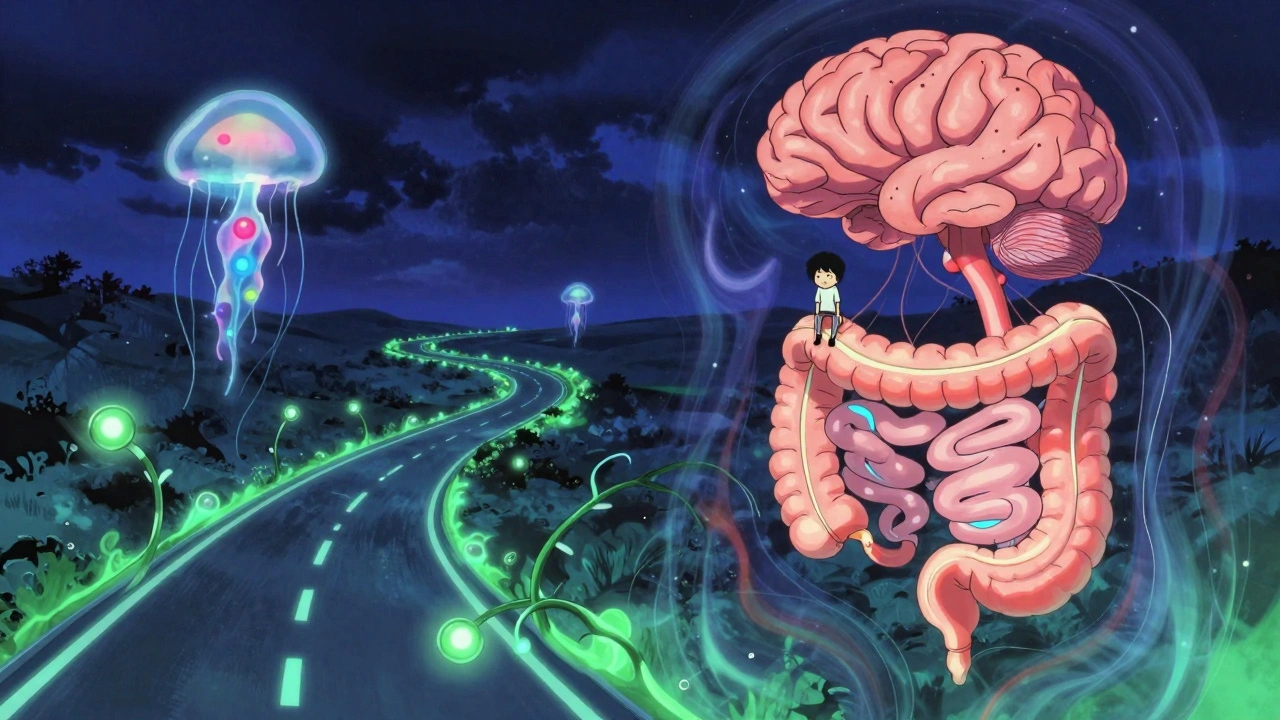
What Exactly Is the Gut-Brain Axis?
The gut-brain axis isn’t a fancy term for stress causing stomach issues. It’s a two-way highway made of nerves, hormones, and immune signals that connect your digestive system to your brain. Your gut has its own nervous system-the enteric nervous system-with over 100 million neurons. That’s more than your spinal cord. It talks to your brain through the vagus nerve, releases serotonin (95% of your body’s serotonin is made in your gut), and sends immune signals that can trigger pain or inflammation.
When this system works right, your gut digests food smoothly, your stress levels stay balanced, and your bowel movements are regular. But in IBS, the line gets crossed. Signals from your gut get amplified in your brain. Your brain starts interpreting normal gut movements as pain. Your stress response stays stuck on high. And your gut microbes-trillions of bacteria living in your intestines-start sending the wrong messages.
How Your Brain Changes When You Have IBS
Brain scans of people with IBS show real, measurable differences. The hypothalamus, which controls stress and digestion, shows more gray matter. The prefrontal cortex, responsible for calming down emotional reactions, shows less. In people with diarrhea-predominant IBS (IBS-D), the areas of the brain that process body sensations get thicker. In constipation-predominant IBS (IBS-C), regions linked to emotional pain shrink.
This isn’t just "feeling anxious." It’s your brain rewiring itself in response to chronic gut signals. That’s why two people with identical symptoms can have completely different experiences-one feels panic with every cramp, the other just feels tired. Your brain’s response to your gut is personal. And it’s not imaginary.
Why Serotonin Is the Missing Link
Most people know serotonin as the "happy chemical"-linked to mood and antidepressants. But in your gut, it’s the traffic controller for bowel movements. Enterochromaffin cells in your intestinal lining make serotonin to tell your gut when to contract and move food along.
In IBS-D, these cells pump out too much serotonin. Studies show levels are nearly 60% higher than in people without IBS. That’s why diarrhea hits fast and hard. In IBS-C, the opposite happens-serotonin drops. Your gut slows down, and stool gets stuck. Even the receptors that respond to serotonin are messed up in 68% of IBS patients. That’s why medications like alosetron (for IBS-D) and prucalopride (for IBS-C) work-they don’t just mask symptoms. They fix the broken signal.

What’s Really Causing Your Symptoms?
It’s not just one thing. IBS symptoms come from a mix of factors:
- Food fermentation: FODMAPs-fermentable carbs in onions, garlic, beans, apples, and wheat-draw water into your gut and get gobbled up by bacteria. The result? Gas, bloating, and pressure that your brain interprets as pain.
- Immune activation: Low levels of natural painkillers like β-endorphin in your gut mean your pain signals aren’t being turned down. Your body’s built-in pain relief system is underpowered.
- Microbiome imbalance: The ratio of Firmicutes to Bacteroidetes bacteria is off in most IBS patients. This isn’t just "bad bacteria." It’s your entire microbial community sending confused signals to your brain.
- Stress response: When you’re anxious, your body shuts down digestion. Your gut slows, your stomach tightens, and your brain becomes hyper-sensitive to any movement. It’s a loop: stress triggers symptoms, symptoms trigger stress.
That’s why a single pill rarely fixes everything. You’re not treating a broken pipe-you’re fixing a broken conversation.
What Actually Works for Relief?
Traditional treatments-antispasmodics, laxatives, anti-diarrheals-only cover the surface. The real breakthroughs target the gut-brain axis directly.
1. Low-FODMAP Diet (50-76% Success Rate)
This isn’t just "eat less beans." It’s a three-phase system: elimination, reintroduction, personalization. You cut out high-FODMAP foods for 4-6 weeks. Then, you slowly add them back one at a time to see what triggers you. Studies show over half of people get major relief. The catch? It’s hard. Most people quit because it’s confusing. Working with a dietitian who knows IBS cuts failure rates in half.
2. Gut-Directed Hypnotherapy (70-80% Response Rate)
This is one of the most powerful tools we have. It’s not stage hypnosis. It’s a structured therapy where you learn to calm your brain’s response to gut signals. In clinical trials, it outperforms medication. People report less pain, fewer bathroom trips, and better sleep. And the effects last-6 months later, most still feel better. The downside? It’s expensive ($1,200-$2,500 for 7-12 sessions) and hard to find. Only one certified practitioner exists for every 500,000 people in rural areas.
3. Probiotics (30-40% Improvement)
Not all probiotics are the same. The strain Bifidobacterium infantis 35624 has the strongest evidence. Taken daily at 1 billion CFUs, it reduces bloating, pain, and bowel urgency better than placebo. Other strains? Mixed results. Stick to the ones backed by research, not the ones on the shelf with cute packaging.
4. Neuromodulation (Emerging but Promising)
Transcutaneous vagus nerve stimulation (tVNS)-a small device placed behind your ear-shows promise. It sends gentle electrical pulses to calm the vagus nerve. Pilot studies report 45-55% reduction in abdominal pain. Larger trials are underway. It’s not FDA-approved yet, but it’s a sign of where things are headed.
Why Most People Stay Stuck
It takes an average of 3-7 years for someone to get an IBS diagnosis. Why? Because doctors still think of it as a gut problem. They test for celiac disease, check for infections, and rule out cancer. But they rarely ask about stress, sleep, or how your gut feels after eating garlic. And when they do, they often give you a quick fix: "Take this pill. Avoid dairy. Come back in six months."
Patients who understand the gut-brain axis stick to treatment 30% longer. They’re more likely to try hypnotherapy or the low-FODMAP diet because they know it’s not "just stress." It’s biology. And when you understand the system, you stop blaming yourself.
The Future Is Personalized
Scientists are now developing tools to map your unique gut-brain profile. The new VisceralSense™ test measures 12 microbial metabolites and serotonin ratios to predict which treatment will work for you. It’s 85% accurate. Clinical trials for new drugs like etrasimod show over 50% symptom improvement in IBS-D patients. The NIH just launched a $15 million project to build personalized treatment algorithms based on your microbiome, brain activity, and stress response.
This isn’t science fiction. It’s happening now. The goal isn’t to cure IBS-it’s to stop treating it like a mystery. We now have the tools to decode it. The challenge? Making these tools accessible to everyone-not just those who can afford $2,500 hypnotherapy or specialized blood tests.
What to Do Right Now
If you have IBS, here’s your starting point:
- Learn the gut-brain connection. Read up. Understand that your symptoms are real, and they’re tied to your nervous system-not your willpower.
- Try the low-FODMAP diet with help. Don’t wing it. Find a registered dietitian who specializes in IBS. The first phase is hard, but it’s worth it.
- Explore gut-directed hypnotherapy. If you can afford it, it’s the most effective long-term solution. If you can’t, look for online programs like The IBS Network’s app or the Monash University app, which has guided sessions.
- Try Bifidobacterium infantis 35624. It’s available as Align or other branded supplements. Give it 4-6 weeks. Track your symptoms.
- Reduce stress daily. Even 10 minutes of breathing, walking, or stretching lowers gut sensitivity. Your nervous system responds to calm.
IBS doesn’t have to be a life sentence. The old model-find the trigger, avoid it, take a pill-is broken. The new model-understand the system, reset the signals, personalize your approach-works. And it’s working for thousands of people right now.
Emily Haworth
December 14, 2025 AT 06:20OMG I JUST REALIZED MY GUT IS TALKING TO MY BRAIN AND IT’S BEEN GIVING ME THE SIDE EYE FOR YEARS 😭🤯
Tom Zerkoff
December 14, 2025 AT 11:21While the article presents a compelling neurobiological framework for understanding irritable bowel syndrome, one must acknowledge the methodological limitations of current microbiome profiling techniques. The assertion that Bifidobacterium infantis 35624 demonstrates superior efficacy requires longitudinal, double-blind, placebo-controlled trials with larger cohorts to establish statistical robustness. Moreover, the commercialization of probiotic formulations often precedes clinical validation, raising ethical concerns regarding consumer misinformation.
Yatendra S
December 15, 2025 AT 12:57if u think ur gut is talking to ur brain… what if ur brain is just listening to the wrong radio station? 🤔 maybe the problem isnt the axis… its the signal. we’ve been taught to fix the body… but what if the body’s been trying to tell us something about the world? capitalism. trauma. silence. maybe your bloating is just your soul screaming for rest.
Webster Bull
December 15, 2025 AT 14:57low fodmap worked for me after 5 years of suffering. no joke. i thought i was just "sensitive"-turns out i was eating onion like it was candy. also, breathing for 10 mins a day? life changer. my gut stopped screaming. my brain finally chillin’.
Lauren Scrima
December 16, 2025 AT 04:53Ohhh so that’s why my therapist said "maybe stop crying in the bathroom" wasn’t a diagnosis? 😏
Himmat Singh
December 17, 2025 AT 21:56It is scientifically untenable to posit that microbial metabolites govern neurological responses without accounting for epigenetic variance across populations. The NIH's $15 million initiative is a classic example of reductionist biomedical hubris. One must consider the sociopolitical context: IBS prevalence is higher in Western societies with high sugar intake and low fiber diversity-factors unrelated to neural signaling. The true etiology lies in dietary colonialism, not serotonin ratios.
Richard Ayres
December 19, 2025 AT 03:13This is one of the most thoughtful summaries of IBS I’ve ever read. It’s easy to feel alone with this condition, especially when doctors dismiss it. But knowing it’s a real, measurable disconnect between gut and brain? That changes everything. I’ve been doing the low-FODMAP diet for three months now-with a dietitian-and my panic attacks before meetings have dropped by 80%. It’s not a cure, but it’s the first time I’ve felt like I’m in control. Thank you for writing this.
nina nakamura
December 19, 2025 AT 22:16Anyone who believes in probiotics as a solution has never read a peer-reviewed paper. The entire microbiome industry is a $50 billion scam built on correlation masquerading as causation. You want relief? Stop eating. Stop stressing. Stop buying supplements. Your gut doesn’t need fixing-it needs silence.
Tyrone Marshall
December 20, 2025 AT 14:26Reading this reminded me of something my grandma used to say: "Your stomach remembers what your mind tries to forget." I spent years thinking my anxiety was just me being dramatic. Turns out, my gut was screaming before my brain even knew there was a problem. I tried hypnotherapy last year. Didn’t think it’d work. I was wrong. It didn’t make the pain go away-but it made me stop fearing it. That’s the real win. You’re not broken. You’re just listening to the wrong frequency. And now? You’ve got the manual.