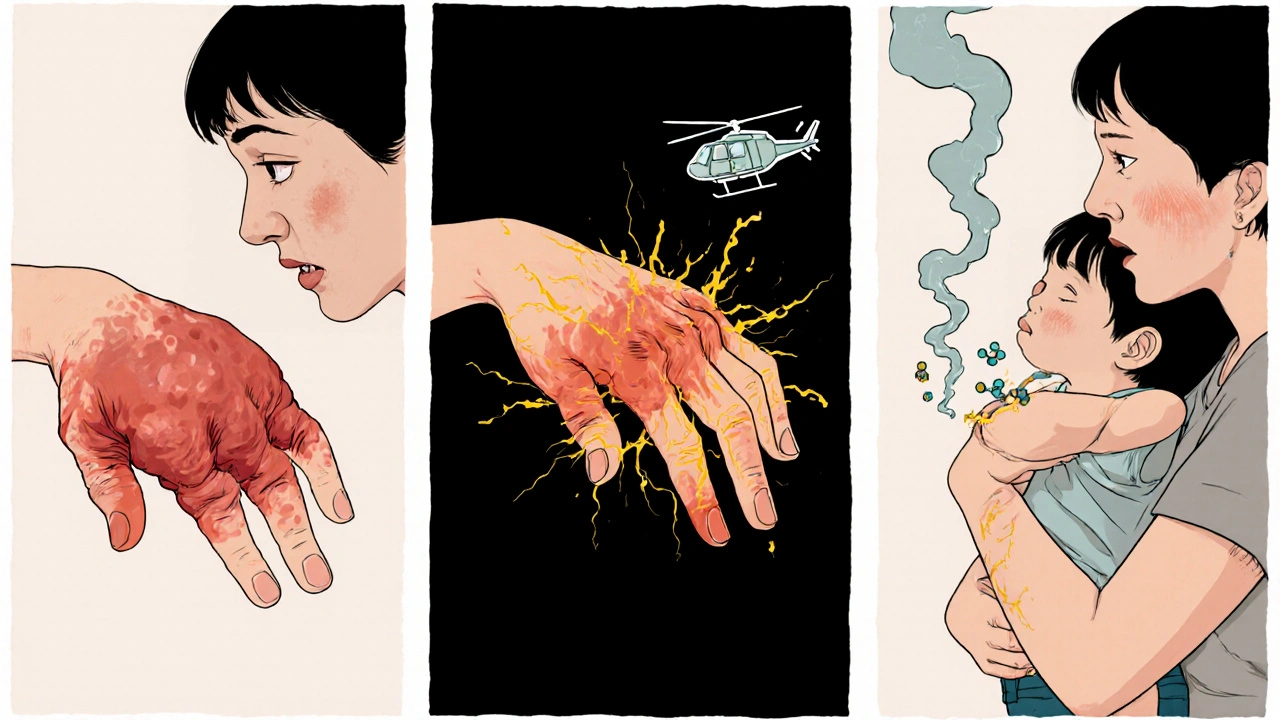
When your immune system turns against your own body, things go wrong fast. That’s what happens in rheumatoid arthritis, psoriatic arthritis, and some other autoimmune conditions. Instead of fighting off germs, your immune cells start attacking your joints, skin, and sometimes even organs. Leflunomide is one of the drugs doctors turn to when other treatments don’t cut it. But how does it actually work inside your body? It’s not just another anti-inflammatory. Leflunomide doesn’t calm the immune system with steroids or blunt it like chemotherapy. It targets a very specific process-one that immune cells need to multiply and cause damage.
What Leflunomide Does Inside Your Cells
Leflunomide works by blocking an enzyme called dihydroorotate dehydrogenase, or DHODH. This enzyme is part of a pathway that makes pyrimidines, which are building blocks for DNA and RNA. Without pyrimidines, cells can’t copy their genetic material and divide. That sounds serious-and it is. But here’s the key: fast-growing immune cells, like the T-cells that drive autoimmune attacks, rely heavily on this pathway. Most other cells in your body can get by on pyrimidines from your diet. Immune cells, especially the ones activated during an autoimmune flare, can’t. They’re forced to make their own.
By shutting down DHODH, leflunomide starves these overactive immune cells of what they need to multiply. It doesn’t kill them outright. It just slows them down enough that they can’t spread the inflammation. Think of it like cutting off fuel to a wildfire. The fire doesn’t vanish immediately, but without new fuel, it can’t grow. Over weeks, the number of attacking T-cells drops, and symptoms like joint swelling and stiffness begin to ease.
Why It’s Different from Other Drugs
Many autoimmune drugs work by suppressing broad parts of the immune system. Methotrexate, for example, affects many rapidly dividing cells, which is why it can cause nausea, low blood counts, or even hair loss. Biologics like adalimumab target specific proteins-TNF-alpha-that trigger inflammation. These drugs are powerful but expensive and often require injections.
Leflunomide is different. It’s a small molecule pill you take once a day. It doesn’t target a single protein or cytokine. Instead, it hits a metabolic bottleneck that only hyperactive immune cells depend on. That’s why it doesn’t hit your red blood cells or gut lining as hard as methotrexate does. It’s more selective. Studies show that after three months of use, people with rheumatoid arthritis see about a 20-30% improvement in joint pain and swelling compared to placebo. That’s not a cure, but it’s meaningful for daily life.
How Long Does It Take to Work?
Don’t expect results overnight. Leflunomide builds up slowly in your bloodstream. It can take four to six weeks before you notice any change. Some people don’t feel real improvement until 12 weeks. That’s because the drug needs time to reduce the population of activated immune cells. Doctors often start patients on a higher dose for the first three days to speed up the buildup-this is called a loading dose. After that, it drops to a maintenance dose of 10 or 20 mg daily.
Because it works so slowly, it’s often combined with other drugs early on. A patient might take leflunomide along with a short course of prednisone to get quick relief while waiting for leflunomide to kick in. This approach is common in clinics and backed by guidelines from the American College of Rheumatology.

Side Effects and What to Watch For
No drug is without risks. The most common side effects of leflunomide are diarrhea, nausea, hair thinning, and elevated liver enzymes. About 1 in 10 people stop taking it because of these issues. Liver function tests are required before starting and every 4-6 weeks during the first six months. If your liver enzymes rise more than three times the normal level, your doctor will likely stop the drug.
Another serious risk is bone marrow suppression. That means your body might make fewer white blood cells, red blood cells, or platelets. If you notice unusual bruising, frequent infections, or extreme fatigue, get your blood checked. Leflunomide also carries a black box warning for fetal harm. It stays in your body for months-even after you stop taking it. Women of childbearing age must use two forms of birth control while on the drug and for at least two years after stopping. Men should also use contraception, since the drug can be present in semen.
There’s a way to remove leflunomide from your system faster if needed. A drug called cholestyramine, usually used for cholesterol, can bind to leflunomide in the gut and help flush it out. In emergencies-like if someone needs surgery or becomes pregnant-this can be life-saving.
Who Shouldn’t Take It?
Leflunomide isn’t for everyone. People with severe liver disease, active infections like hepatitis B or C, or those with severely weakened immune systems should avoid it. If you’ve had a bad reaction to similar drugs like teriflunomide (used for multiple sclerosis), you’re likely not a candidate. It’s also not approved for children under 18, because long-term effects on growing immune systems aren’t fully known.
People with kidney disease may need a lower dose. The drug is processed by the liver, but its active metabolite is cleared by the kidneys. If your kidneys aren’t working well, levels can build up, increasing side effect risks. Your doctor will check your kidney function before prescribing it.
What Happens When You Stop?
Stopping leflunomide doesn’t mean your symptoms come back immediately. But over time, the immune system can rebound. Studies show that within 6-12 months of stopping, about half of patients see a return of joint pain and swelling. That’s why many people stay on it for years-even decades-if it’s working and their liver and blood counts stay normal.
If you do stop, don’t just quit cold turkey. Talk to your doctor. They might suggest switching to another disease-modifying drug like sulfasalazine or a biologic to keep the disease under control. Abruptly stopping can lead to a flare that’s harder to manage.
Real-World Use and What Patients Say
In clinics across Australia, Europe, and the U.S., leflunomide is still widely prescribed-not because it’s flashy, but because it’s reliable. A 2023 study of over 1,200 rheumatoid arthritis patients found that 68% stayed on leflunomide for at least two years. The main reason? It worked. The main reason people stopped? Side effects, not lack of effectiveness.
One patient in Melbourne, 56, started leflunomide after methotrexate gave her severe mouth sores. Within three months, her swollen knuckles softened. She still gets morning stiffness, but she can now open jars, drive, and play with her grandchildren again. She takes her pill every night with a glass of water and gets blood tests every six weeks. It’s not perfect-but it’s hers.
Alternatives and Where Leflunomide Fits Today
There are more options now than ever. Biologics like etanercept or JAK inhibitors like tofacitinib work faster and are often more effective. But they cost 10 to 20 times more. In countries with public healthcare, leflunomide remains a first-line choice for moderate disease because it’s affordable, effective, and oral.
It’s also used off-label for psoriatic arthritis and lupus-related joint issues. In some cases, it’s combined with low-dose methotrexate for a dual attack on the immune system. This combo is common in Australia’s public hospitals, where cost and access matter.
Leflunomide isn’t the newest drug. But it’s not outdated either. It’s a quiet, steady player in the autoimmune treatment toolbox. For many, it’s the difference between living with pain and living with control.
How long does it take for leflunomide to start working?
It usually takes 4 to 6 weeks to notice any improvement, and full effects can take up to 12 weeks. This is because the drug needs time to build up in your system and reduce the number of overactive immune cells. Doctors often start with a higher dose for the first few days to speed this up.
Can leflunomide cause liver damage?
Yes, it can. Leflunomide may raise liver enzyme levels, which can signal liver stress. That’s why regular blood tests are required-every 4 to 6 weeks during the first six months. If levels go above three times the normal range, the drug is usually stopped. People with existing liver disease shouldn’t take it.
Is leflunomide safe during pregnancy?
No. Leflunomide can cause serious birth defects. It stays in your body for months-even after you stop taking it. Women must use two forms of birth control while on the drug and for at least two years after stopping. Men should also use contraception, as the drug can be present in semen. If pregnancy occurs, a special washout procedure with cholestyramine can help remove it faster.
What are the most common side effects?
The most common side effects are diarrhea, nausea, hair thinning, and elevated liver enzymes. About 1 in 10 people stop taking it because of these issues. Less common but more serious risks include low blood cell counts, which can lead to infections or unusual bruising. Regular blood tests help catch these early.
Can I take leflunomide with other arthritis medications?
Yes, it’s often combined with other drugs. Many patients take it with low-dose methotrexate or a short course of prednisone to get faster symptom relief. It’s also used alongside NSAIDs for pain control. But combining it with other immune-suppressing drugs increases infection risk, so your doctor will monitor you closely.
What happens if I stop taking leflunomide?
Symptoms may return within 6 to 12 months. Leflunomide doesn’t cure autoimmune disease-it controls it. Stopping suddenly can lead to a flare that’s harder to manage. If you need to stop, talk to your doctor about switching to another disease-modifying drug to keep your condition stable.
Is leflunomide better than methotrexate?
It depends on the person. Methotrexate works faster and is often the first choice, but it can cause mouth sores, nausea, and liver issues. Leflunomide is easier on the stomach for some and doesn’t require injections. It’s often chosen when methotrexate isn’t tolerated. Both are equally effective long-term, but side effect profiles differ.

Uttam Patel
October 29, 2025 AT 08:33Leflunomide? More like leflunomind. You take this pill and suddenly your hair thinks it’s on vacation. But hey, at least your joints aren’t screaming anymore. I’ll take thinning hair over crippling pain any day.
Kirk Elifson
October 31, 2025 AT 05:21Why are we even talking about this third-world drug when we have fancy biologics? In America we don’t take pills that make your liver whisper sweet nothings to your kidneys. This is why healthcare’s broken-people settle for scraps when they could have steak.
Nolan Kiser
November 1, 2025 AT 17:18For those wondering how selective leflunomide really is-it’s actually brilliant. Most cells get pyrimidines from food, but activated T-cells are metabolic junkies that have to make their own. By hitting DHODH, you’re not nuking the whole immune system, just starving the overeagers. That’s why side effects are milder than methotrexate. It’s precision medicine before it was cool.
Yaseen Muhammad
November 1, 2025 AT 20:34It’s important to note that leflunomide’s active metabolite, A77 1726, has a half-life of up to 18 days. This explains the delayed onset and the necessity of a loading dose. Also, while liver monitoring is standard, many clinicians overlook the need to check renal function regularly, especially in patients with borderline kidney health. Always confirm eGFR before and during therapy.
Dylan Kane
November 1, 2025 AT 21:28So let me get this straight-you’re telling me I have to take a pill that could wreck my liver, ruin my hair, and still not fix my arthritis… but I have to use TWO forms of birth control for TWO YEARS? And if I get pregnant? Oh, I guess I’ll just chug cholestyramine like it’s a protein shake. Yeah, I’ll pass. This is why I’m switching to CBD oil.
KC Liu
November 3, 2025 AT 07:21Did you know the FDA approved leflunomide after a single Phase II trial? And that the original patent holder was a German pharma company that later got bought by a Chinese conglomerate? No one talks about this. But if you dig into the FDA’s 2004 advisory committee minutes, you’ll see the data was borderline. They approved it because they had no alternatives. That’s not medicine. That’s desperation.
Shanice Alethia
November 3, 2025 AT 22:51My aunt took this for 7 years. She lost her hair, her job, her marriage, and then her liver. They told her it was "manageable." Manageable? My aunt now lives in a nursing home because her immune system collapsed after they tried to wean her off. This drug is a slow-motion suicide pact disguised as treatment. Don’t be fooled by the "quiet player" nonsense-it’s a silent killer with a pill bottle.
shridhar shanbhag
November 4, 2025 AT 00:57For those in India or other countries where biologics are unaffordable, leflunomide remains a lifeline. I’ve seen patients with severe RA go from wheelchair to walking with a cane in 4 months. Yes, side effects happen. But we monitor, we adjust, we educate. It’s not perfect-but neither is poverty. This drug gives dignity to people who otherwise have no options.
Eben Neppie
November 5, 2025 AT 14:10Anyone who says leflunomide is outdated hasn’t looked at real-world data from the UK’s NICE guidelines or Australia’s PBS. It’s still a first-line DMARD in public systems because it works, it’s cheap, and it’s oral. Biologics are flashy, but they’re not better for everyone. In fact, over half of patients on biologics still need a backup DMARD. Leflunomide is that backup-and it’s earned its place.
Hudson Owen
November 5, 2025 AT 17:03I appreciate the thoroughness of this post. The distinction between metabolic targeting and cytokine blockade is crucial for understanding why leflunomide occupies a unique niche. The emphasis on monitoring liver enzymes and renal function reflects responsible clinical practice. I only wish more patients were educated on the importance of adherence and the rationale behind the delayed onset-it reduces frustration and abandonment.
Steven Shu
November 7, 2025 AT 10:01I’ve been on it for 3 years. Diarrhea sucked for the first month, but it faded. Hair got thinner, but I wear hats now. Liver tests are fine. I can hold my grandkids without wincing. It’s not glamorous, but it’s mine. If you’re on methotrexate and your mouth is raw from sores, give this a shot. Just don’t skip the bloodwork.
Milind Caspar
November 9, 2025 AT 02:33Let’s be honest-leflunomide is a Trojan horse. The pharmaceutical industry knows it’s metabolized by the liver and excreted by the kidneys, so they market it as "selective" while quietly relying on patients’ ignorance of pharmacokinetics. The black box warning for fetal harm? That’s not a side effect-it’s a liability hedge. And the cholestyramine washout? That’s not a safety feature-it’s a legal loophole. This drug was designed to be profitable, not compassionate.
Rose Macaulay
November 9, 2025 AT 12:03My mom’s on it. She’s 68. She cried when she could finally button her blouse again. I know the risks. We do the bloodwork. We talk to her doctor. It’s not perfect, but it’s given her back pieces of her life. That’s worth more than any side effect list.