Medication Matchmaker: Find Your Best Diltiazem Alternative
How important is heart rate control for you?
Do you experience or worry about swelling (edema)?
Are you taking medications that interact with CYP3A4?
Do you have prostate enlargement or BPH?
Recommended Alternatives
Based on your responses, we recommend considering the following options:
When you hear the name Diltiazem is a calcium‑channel blocker used to treat high blood pressure, angina, and certain heart rhythm issues. If you’re looking for Diltiazem alternatives, you’ve come to the right place. This guide walks through the most common substitutes, how they stack up, and which situation calls for each.
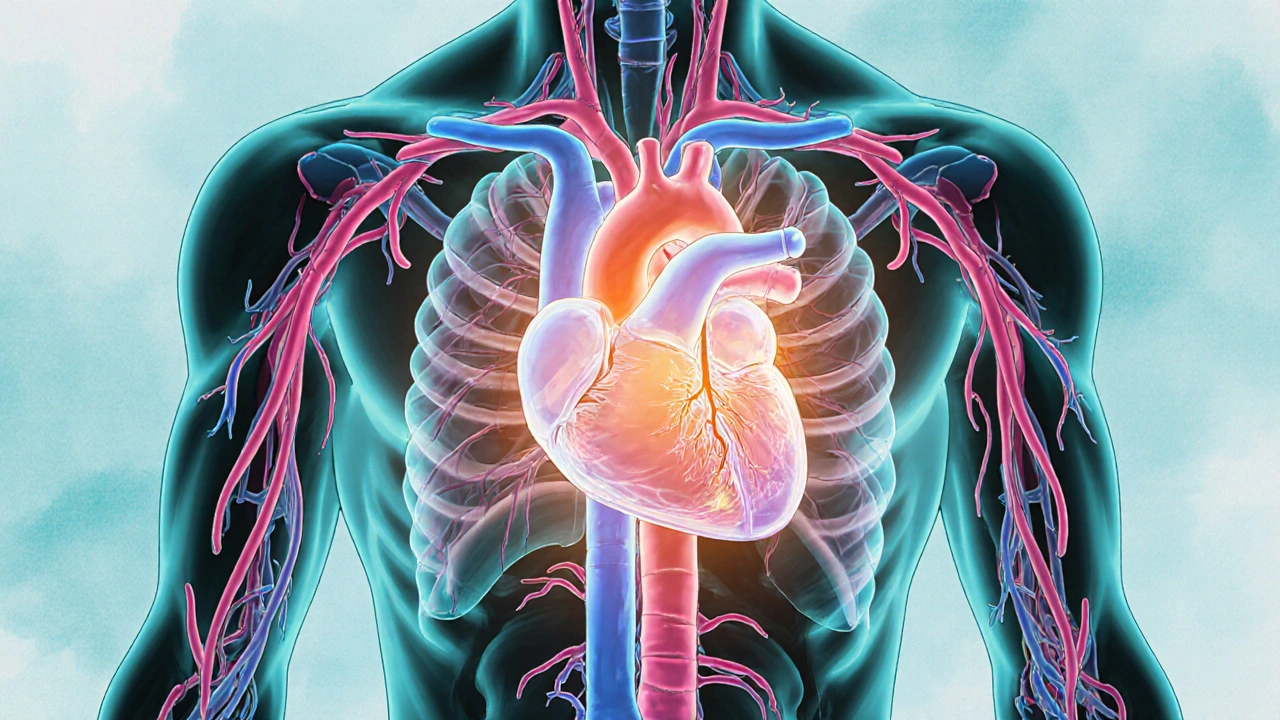
How Diltiazem Works
Diltiazem belongs to the non‑dihydropyridine class of calcium‑channel blockers. By relaxing the smooth muscle in blood vessels and slowing electrical conduction in the heart, it lowers blood pressure and eases chest pain. The effect lasts about 6‑8 hours for the standard tablet, which means most patients take it once or twice daily.
When You Might Need an Alternative
Even a solid drug like Diltiazem isn’t the best fit for everyone. Common reasons to switch include:
- Side‑effects such as swelling, constipation, or a slow heart rate that don’t improve with dosage tweaks.
- Drug interactions - Diltiazem can boost levels of certain statins or anti‑arrhythmics, creating a safety headache.
- Specific medical conditions - patients with severe heart failure may need a different approach.
- Insurance formularies - sometimes a cheaper drug gets preferential coverage.
Top Alternatives to Consider
Below are the most frequently prescribed substitutes. Each belongs to a related drug class but has its own quirks.
Verapamil is another non‑dihydropyridine calcium‑channel blocker, often chosen for its stronger effect on heart rate control.
Amlodipine is a dihydropyridine calcium‑channel blocker that focuses more on vessel dilation, making it a go‑to for hypertension without big impacts on heart rhythm.
Nifedipine is also a dihydropyridine, known for quick onset and often used in acute angina management.
Doxazosin belongs to the alpha‑blocker family, providing vasodilation without directly affecting calcium channels.
Labetalol is a mixed alpha‑ and beta‑blocker, useful when both blood pressure and heart rate need simultaneous control.

Head‑to‑Head Comparison Table
| Drug | Class | Primary Use | Typical Dose Range | Impact on Heart Rate | Common Side‑effects |
|---|---|---|---|---|---|
| Diltiazem | Non‑dihydropyridine CCB | Hypertension, angina, atrial fibrillation | 30‑120 mg daily | Decreases (moderate) | Edema, constipation, dizziness |
| Verapamil | Non‑dihydropyridine CCB | Rate control for SVT, angina | 80‑480 mg daily | Decreases (strong) | Constipation, bradycardia, gum hypertrophy |
| Amlodipine | Dihydropyridine CCB | Essential hypertension | 2.5‑10 mg daily | Little effect | Peripheral edema, headache |
| Nifedipine | Dihydropyridine CCB | Acute coronary syndrome, hypertension | 10‑90 mg daily (SR) | Little effect | Flushing, reflex tachycardia |
| Doxazosin | Alpha‑1 blocker | Benign prostatic hyperplasia, hypertension | 1‑8 mg daily | Neutral | First‑dose hypotension, dizziness |
Choosing the Right Option for You
Think of the selection process as a short questionnaire:
- Do you need strong heart‑rate control? If yes, Verapamil or Labetalol often win.
- Is peripheral edema a big concern? Amlodipine may actually worsen it, while Diltiazem’s edema is usually milder.
- Are you on medications that interact with CYP3A4? Diltiazem and Verapamil share that pathway; Amlodipine has fewer interactions.
- Do you have prostate enlargement? Doxazosin hits two birds with one stone - it lowers pressure and eases urinary flow.
- What does your insurance cover? Check the formulary; sometimes a generic version of Amlodipine is cheaper than brand‑name Diltiazem.
Answering these questions gives a clear direction, but always run the final choice by your prescriber.
Safety, Interactions, and Monitoring
Every heart drug carries a monitoring checklist. Below are the top points for Diltiazem and its rivals.
- Blood pressure and heart rate: Check at baseline, then after the first week, and quarterly.
- Liver function: Diltiazem is metabolized by the liver; abnormal enzymes may require dose adjustments.
- Drug‑drug interactions: Combine with beta‑blockers cautiously; avoid simultaneous use with strong CYP3A4 inhibitors like clarithromycin.
- Electrolytes: Potassium and magnesium levels matter for arrhythmia risk, especially when using Verapamil.
- Pregnancy: Category C - only use if benefits outweigh risks.
Practical Tips for Switching
Switching isn’t just swapping pills - timing matters.
- Discuss the plan with your doctor; they’ll calculate an equivalent dose.
- Most alternatives need a short overlap period (24‑48 hours) to avoid blood‑pressure spikes.
- Keep a symptom log for at least two weeks to track any new side‑effects.
- Know the “red‑flag” signs: sudden dizziness, chest pain, or a heartbeat that feels too slow or too fast.
- Schedule a follow‑up blood‑pressure check within a week of the change.
Key Takeaways
- Diltiazem is a solid all‑rounder for blood pressure, angina, and rhythm control.
- Verapamil offers stronger heart‑rate slowing, ideal for certain arrhythmias.
- Amlodipine shines when you need pure blood‑pressure reduction without heart‑rate effects.
- Nifedipine works fast for acute chest pain but can cause reflex tachycardia.
- Alpha‑blockers like Doxazosin are useful when prostate issues coexist with hypertension.
- Always match the drug to your specific health goals, other meds, and insurance coverage.
Frequently Asked Questions
Can I take Diltiazem with a beta‑blocker?
Yes, but only under close medical supervision. The combo can lower heart rate too much, so your doctor will watch the pulse and may adjust doses.
Why does Diltiazem cause ankle swelling?
The drug widens blood vessels, causing fluid to leak into surrounding tissues, especially in the lower legs. Elevating the feet and reducing sodium intake can help.
Is Amlodipine safer for older adults?
Amlodipine’s gentle effect on heart rate makes it a common first‑line choice for seniors, but watch for swelling. Dose starts low (2.5 mg) and titrates up.
What should I do if I miss a Diltiazem dose?
Take it as soon as you remember unless it’s almost time for the next dose. In that case, skip the missed one-don’t double up.
Are there any foods I should avoid with Diltiazem?
Grapefruit juice can raise Diltiazem levels, increasing side‑effects. It’s best to limit or avoid it while on the medication.
How quickly does Verapamil start working?
Immediate‑release forms can lower heart rate within an hour, while extended‑release tablets reach a steady effect after 2‑3 days.
Can I use Doxazosin for hypertension alone?
Yes, Doxazosin is approved for high blood pressure, but many doctors prefer it when prostate enlargement is also present because it treats both.
Poornima Ganesan
October 18, 2025 AT 20:32Diltiazem indeed sits at the crossroads of hypertension, angina, and rhythm management, and its pharmacology merits a thorough dissection. First, the drug’s non‑dihydropyridine backbone confers a dual action that many prescribers overlook when they simply label it a “blood pressure pill.” Its half‑life of six to eight hours dictates a dosing schedule that can be conveniently once‑daily for many, yet the same kinetic profile also creates peaks that may precipitate edema in susceptible individuals. Moreover, the cytochrome P450 3A4 pathway that metabolizes Diltiazem introduces a cascade of drug‑drug interactions that often go unmentioned in patient handouts. For instance, concomitant use with certain statins can raise plasma concentrations of the lipid‑lowering agents, potentially leading to myopathy. The same metabolic route also amplifies the levels of some anti‑arrhythmics, a fact that cardiologists should flag during chart reviews. When clinicians consider alternatives, they must weigh not only efficacy but also the side‑effect spectrum that each class brings. Verapamil, while sharing the non‑dihydropyridine skeleton, exerts a stronger negative dromotropic effect, making it preferable for atrial flutter but riskier for patients with existing conduction disease. Amlodipine’s dihydropyridine profile spares heart‑rate modulation, yet its propensity for peripheral edema can rival that of Diltiazem if the dose is escalated too quickly. Nifedipine, especially in its immediate‑release form, can cause reflex tachycardia, a paradoxical response that may aggravate ischemic chest pain rather than relieve it. Alpha‑blockers such as Doxazosin bring the benefit of prostate symptom relief, but their first‑dose hypotension is notorious, demanding careful titration. Labetalol offers a hybrid alpha‑beta blockade, useful in hypertensive emergencies, yet its dosing complexity can confuse outpatient management. Insurance formulary constraints often act as the hidden decision‑maker, nudging prescribers toward generic options that may not be pharmacologically optimal for a given patient’s comorbidities. The practical tip of maintaining a symptom log after a switch cannot be overstated, because subtle changes in dizziness or ankle swelling may signal the need for dose adjustment. Finally, any transition should be anchored by a follow‑up blood‑pressure check within a week, because the hemodynamic impact of switching from a non‑dihydropyridine to a dihydropyridine is not always linear. In summary, the choice between Diltiazem and its alternatives is a multidimensional puzzle that blends pharmacology, patient preference, and health‑system economics, and overlooking any piece can compromise therapeutic success.
Emma Williams
October 23, 2025 AT 08:13Great summary of the options
Stephanie Zaragoza
October 27, 2025 AT 22:20The guide meticulously delineates each drug class, yet it could benefit from a clearer hierarchy of contraindications, especially regarding CYP3A4 substrates; while the table is comprehensive, the absence of explicit dosing conversion factors between Diltiazem and Verapamil may perplex junior prescribers; furthermore, the discussion of peripheral edema lacks quantitative incidence rates, which would enable a more evidence‑based comparison; I also noted that the renal function considerations were briefly mentioned, but a deeper analysis of dose adjustments in chronic kidney disease stages would be advantageous; overall, the article succeeds in presenting a balanced view, though a few additional caveats would elevate its clinical utility.
Mike Hamilton
November 1, 2025 AT 13:26Diltiazem works by relaxin the muscles in the blood vessels. It helps to lower the blood presure and eases chest pain. If you cant tke it cause of side effects, there are othr options like verapamil or amlodipine. Talk to your doc to see which one suits you best, they will check your health record. Switching meds is not just a swap, you need to monitor your bp and heart rate for a while.
Liberty Moneybomb
November 6, 2025 AT 04:33The moment you step into the pharmacy and see a brand‑name like Diltazem, you’re already playing into a clandestine script written by the drug lords of Big Pharma. They parade Verapamil and Amlodipine as harmless alternatives, yet each tablet is laced with hidden profit motives that the average consumer never sees. Even the humble Doxazosin, marketed for prostate health, carries a silent clause in its approval papers that binds you to a lifetime of follow‑up visits. So before you trust any of these “top alternatives,” remember that your blood pressure is a lever in a larger game of control. The truth may be uncomfortable, but awareness is the only antidote to the manipulation.
Grace Hada
November 10, 2025 AT 19:40If you can’t tolerate the swelling, drop Diltiazem immediately. Anything else is just a marketing gimmick.
Fabian Märkl
November 15, 2025 AT 10:46Hey Liberty, I get where you’re coming from 😊 – the pharma landscape can feel overwhelming, but the data we have today does show real benefits for many patients, so it’s worth discussing options with a cardiologist who can tailor the choice to your specific needs 👍
Natala Storczyk
November 20, 2025 AT 01:53Seriously, Stephanie, your critique is so painfully pedantic!!! You’re ignoring the fact that the American healthcare system thrives on these very “caveats” we’re forced to acknowledge; the over‑reliance on tables misses the human element that only our great nation’s physicians truly understand!!!
nitish sharma
November 24, 2025 AT 17:00Dear colleagues, I appreciate the thorough analysis presented herein and would like to add that patient education, particularly regarding the potential for grapefruit‑juice interactions, remains a cornerstone of safe Diltiazem utilisation. Moreover, ensuring that follow‑up appointments are scheduled promptly can mitigate adverse events.
Rohit Sridhar
November 29, 2025 AT 08:06Reading this guide gave me confidence that switching from Diltiazem to another agent can be a smooth journey. The clear tables make it easy to compare side‑effect profiles, and I especially liked the tip about keeping a symptom log. It’s reassuring to know that alternatives like Amlodipine or Verapamil are readily available if insurance becomes an obstacle. I also appreciate the practical advice on timing the overlap period – that detail often gets lost in other articles. With this information, patients can feel empowered to discuss options openly with their doctors.
Brian Van Horne
December 3, 2025 AT 23:13The exposition strikes a fine balance between clinical rigor and readability; kudos to the author. A splash of vivid terminology adds flavor without sacrificing precision.
Norman Adams
December 8, 2025 AT 14:20Oh, brilliant, another exhaustive comparison that will surely change the world of antihypertensives. As if clinicians didn’t already have enough spreadsheets to fill.
Margaret pope
December 13, 2025 AT 05:26Thanks for sharing this guide it’s really helpful for patients who are confused. Keep adding more practical tips and we’ll all benefit