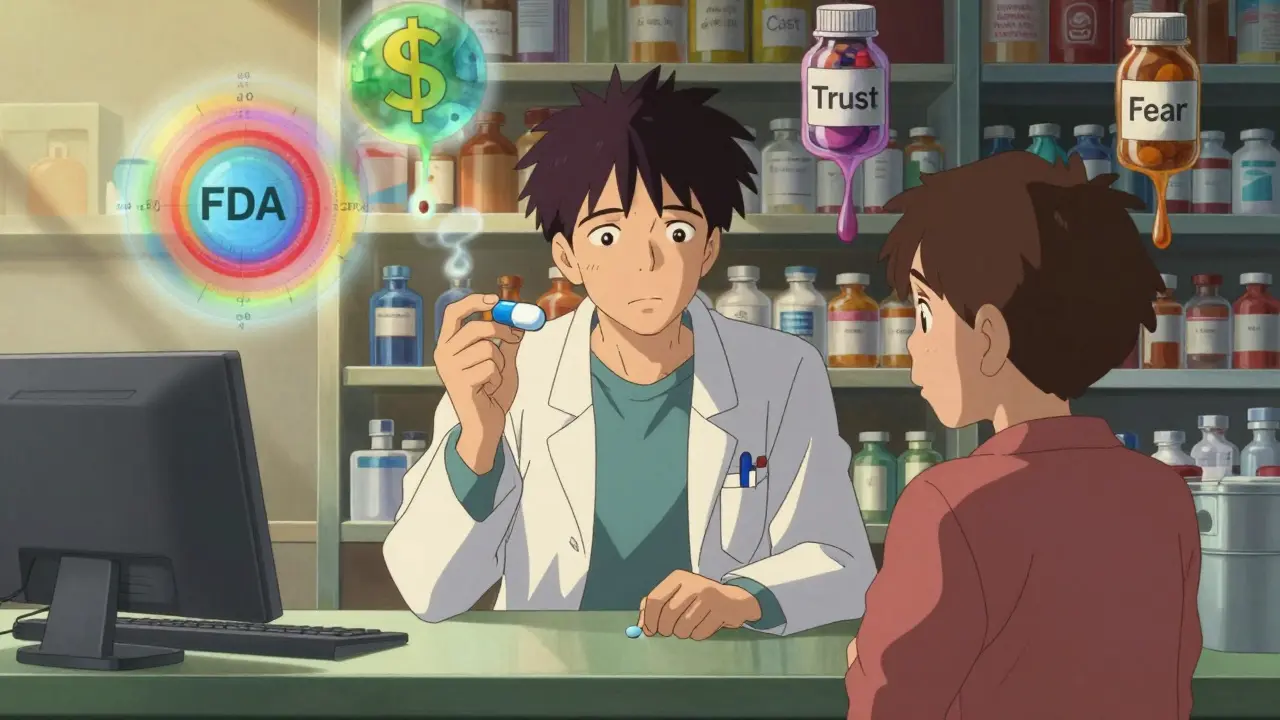
Every day, pharmacists face a quiet but persistent challenge: convincing patients that a small, differently colored pill is just as safe and effective as the brand-name drug their doctor prescribed. It’s not just about saving money. It’s about trust, communication, and clinical judgment - all squeezed into a 90-second counseling window between prescriptions.
Why Pharmacists Care So Much About Generic Substitution
Generic substitution isn’t just a cost-cutting trick. It’s a legally backed practice rooted in the 1984 Hatch-Waxman Act, designed to let pharmacists swap a brand-name drug for a generic version that’s proven to work the same way. The FDA requires these generics to match the original in active ingredients, strength, dosage form, and route of administration. Bioequivalence? They must deliver the same amount of medicine into the bloodstream within a narrow range - 80% to 125% of the brand. That’s not guesswork. It’s science. But here’s the catch: even though 96% of eligible prescriptions are candidates for substitution, and 70% of pharmacists say it improves their role in patient care, nearly half still struggle to make it work smoothly. Why? Because the system doesn’t always account for human factors - patient fears, physician silence, and the messy reality of daily pharmacy life.Patient Doubts Are the Biggest Hurdle
Patients aren’t being difficult on purpose. They’re confused. And it’s not their fault. Many see the lower price and assume the drug is cheaper because it’s weaker. Some notice the pill looks different - smaller, rounder, a different color - and think it’s not the same medicine. Others remember a time when a generic didn’t seem to work as well, even if it was a coincidence. A third of patients report negative experiences after switching, and those stories stick. In Australia, pharmacists spent extra time explaining generics to patients with dementia, mental illness, or those taking five or more medications. In Italy and the U.S., patients often asked to call their doctor before accepting the switch. That’s not just inconvenient - it’s a workflow breaker. One study found 50% of patients requested physician approval before taking a generic. But here’s the problem: 64% of those patients never heard about substitution from their doctor in the first place. So now, the pharmacist is stuck being the educator, the negotiator, and the reassurer - all while juggling ten other patients.The NTI Problem: When Substitution Gets Risky
Not all drugs are created equal when it comes to substitution. Narrow therapeutic index (NTI) drugs are the tricky ones. These are medications where even a tiny change in blood levels can mean the difference between effectiveness and danger. Think anti-seizure drugs like phenytoin or levetiracetam. Or blood thinners like warfarin. Or thyroid meds like levothyroxine. For these, the FDA’s 3.5% average absorption difference might sound small - and it is, statistically. But in practice, a 10% fluctuation in blood levels can trigger a seizure, a clot, or a thyroid crisis. Pharmacists know this. That’s why many hesitate to substitute NTI drugs unless the patient is stable, the prescriber is on board, and the patient fully understands the risk. Some states even have rules banning automatic substitution for certain NTI medications. But not all do. And when a patient walks in with a prescription for levetiracetam and the brand is out of stock, the pharmacist has to decide: do I swap it? Do I call the doctor? Do I risk a bad outcome just to save $20?Doctors Aren’t Helping - And That’s Making Things Worse
Here’s something most patients don’t know: their doctor rarely talks to them about generics. In fact, only 38.5% of patients are told they can refuse a generic substitution. And only 52% are told how much money they’ll save. Doctors assume pharmacists will handle it. Pharmacists assume doctors already explained it. Meanwhile, the patient gets a pill they don’t recognize and walks away with unanswered questions. Studies show that when doctors mention generics during the visit - even just saying, “This generic works just like the brand, and it’ll cut your bill in half” - patient acceptance jumps. But that rarely happens. So pharmacists are left holding the bag. They’re the ones explaining why a pill that looks like a blue marble is just as good as the white capsule with the logo. And they’re doing it without the authority of the prescriber’s voice backing them up.Education Is the Real Solution - But It’s Not Easy
The good news? Education works. One study found that after a simple 2-minute conversation explaining FDA bioequivalence standards, patient acceptance of generics rose dramatically. Pharmacists who used the 3.5% absorption difference statistic - “The medicine in this pill is almost exactly the same as the brand, within a margin the FDA considers safe” - saw fewer refusals. But here’s the problem: most pharmacies don’t have time for 2-minute conversations. The average counseling time per prescription is under 90 seconds. And if the patient is in a hurry, stressed, or doesn’t speak English well, the conversation gets cut short. Some pharmacies have started using printed handouts with simple icons: a scale showing “same medicine,” a checkmark for “FDA-approved,” and a dollar sign for “save money.” Others train staff to use phrases like, “This is the same active ingredient, just made by a different company.” But these tools aren’t universal. And they’re not always used consistently.
What Pharmacists Wish They Could Change
If pharmacists could rewrite the rules, here’s what they’d ask for:- Doctors should mention generics during the visit. Not a footnote. Not a handout. A direct conversation: “I’m prescribing this generic because it’s just as good and will save you money.”
- Patients should get a clear right to refuse. Right now, only 38.5% are told they can say no. That’s not informed consent - that’s an oversight.
- State laws should clarify substitution rules for NTI drugs. No more guessing. Clear guidelines for when substitution is allowed, when it’s not, and when you need to call the prescriber.
- Pharmacists need better tools. Not just handouts - digital prompts in the pharmacy system that flag NTI drugs, remind staff to counsel, and suggest simple phrases for patient conversations.
It’s Not About Saving Money - It’s About Trust
Generic substitution isn’t just a pharmacy practice. It’s a test of the entire healthcare system’s ability to communicate clearly and build trust. Pharmacists aren’t trying to replace brand-name drugs because they hate them. They’re trying to make care more affordable and accessible. But they can’t do it alone. Patients need to understand that a generic isn’t a “cheap version.” It’s a scientifically validated alternative. Doctors need to step up and say so. And the system needs to give pharmacists the time and tools to make that conversation happen. Right now, the system is broken in small but meaningful ways. A patient refuses a generic because they don’t trust it. A pharmacist skips counseling because they’re behind. A doctor never mentions it because they assume it’s handled. And the result? Poor adherence, avoidable hospital visits, and wasted money. The solution isn’t more regulation. It’s better communication. One conversation at a time.Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove bioequivalence - meaning they deliver the same amount of medicine into the bloodstream within a 80-125% range of the brand. Over 2,000 studies show an average absorption difference of just 3.5%, which is considered clinically insignificant for most medications.
Why do generic pills look different from brand-name pills?
By law, generic manufacturers can’t copy the exact appearance of brand-name pills because that would violate trademark rules. So generics may differ in color, shape, size, or markings - but the active ingredient and how it works in your body are the same. These differences are purely cosmetic and don’t affect safety or effectiveness.
Can pharmacists substitute any drug with a generic?
Most can - but not all. Drugs with a narrow therapeutic index (NTI), like warfarin, levothyroxine, or anti-seizure medications, require extra caution. Some states restrict automatic substitution for these. Pharmacists may need to consult the prescriber or get patient consent before switching. Always check local laws and clinical guidelines.
Why do some patients refuse generic substitution?
Common reasons include lack of knowledge, distrust in generic manufacturers (especially if they’re overseas), confusion over changing pill appearance, or past negative experiences - even if unrelated. Some patients believe cheaper means lower quality. Others fear switching will disrupt their treatment. Education and clear communication from pharmacists can reduce these fears.
What should I do if my pharmacist switches my medication without telling me?
You have the right to ask. Before leaving the pharmacy, check the label and pill appearance. If it’s different from what you’re used to, ask: “Is this a generic?” and “Was I told I could refuse this?” You can always request the brand-name drug - though you may pay more. If you’re uncomfortable, call your doctor to confirm the switch is appropriate.
Do pharmacists make more money by prescribing generics?
No. Pharmacists don’t earn more from dispensing generics. Their profit margin is often smaller on generics because they cost less overall. The incentive for substitution isn’t financial - it’s clinical and systemic. Pharmacists support generics because they help patients afford their medicine, reduce waste, and improve adherence - not because they get paid more.
Karen Conlin
January 23, 2026 AT 03:18Look, I get why people freak out about generic pills looking different. But here’s the thing: the FDA doesn’t mess around. If it’s approved, it works. I’ve been a pharmacist for 18 years and I’ve seen patients switch from brand-name Lamictal to generic and never have a seizure. The color change? That’s just trademark law. The active ingredient? Identical. Stop letting fear drive your health decisions.
And yes, doctors should say something. But until they do, we’re stuck being the ones to explain it while you’re rushing out the door with your 10 prescriptions. We’re not trying to save money-we’re trying to keep you alive and not bankrupt.
Also, if you think overseas manufacturers are sketchy, you should see how many brand-name pills are made overseas too. The system’s broken, not the pills.
asa MNG
January 23, 2026 AT 08:09bro i swear i took a generic adderall once and i felt like my brain was wrapped in saran wrap 😵💫 i was zoned out for 3 hours like what the actual f*** is this?? brand name got me back on track. maybe the generics are just bad?? 🤔 maybe big pharma is hiding something?? 🕵️♂️
Sushrita Chakraborty
January 23, 2026 AT 18:07It is a matter of profound concern that the burden of patient education is being placed entirely upon pharmacists, who operate under severe time constraints and without the authority of the prescribing physician. The Hatch-Waxman Act, while commendable in intent, has created a systemic imbalance wherein the clinical responsibility for communication is outsourced to a profession that is neither compensated nor empowered to perform it adequately. This is not merely an operational inefficiency-it is an ethical failure of the healthcare ecosystem.
Josh McEvoy
January 24, 2026 AT 16:16so like… what if the generic makes you feel like you’re slowly turning into a zombie? 😭 i mean i didn’t ask for this. i asked for my blue pill. now i’m holding a yellow one and i’m just… confused. why does this have to be so dramatic? i just want to feel normal.
also i think the FDA is just trying to save money. they don’t care if we’re okay.
pls help
Heather McCubbin
January 26, 2026 AT 10:44Let’s be real. The system is rigged. You think the FDA really tests every single generic? Nah. They rubber stamp it because corporations pay them off. I know a guy whose cousin’s neighbor took a generic thyroid med and ended up in the ER. That’s not a coincidence. That’s a pattern. And your doctor? They don’t care. They’re on a clock. The pharmacist? They’re just trying to get you out the door so they can go to their next shift.
People are dying because we’ve turned medicine into a commodity. And now you’re telling me to trust a pill that looks like a gummy bear? I’d rather pay extra and sleep at night.
Wake up people. This isn’t science. It’s capitalism.
Tiffany Wagner
January 26, 2026 AT 23:24My grandma switched to generic levothyroxine last year and her TSH stayed perfect. She didn’t even notice. But she also had the pharmacist sit with her for 5 minutes and explain it with pictures. Maybe it’s not about the pill. Maybe it’s about the time someone takes to care.
I wish more pharmacies did that.
Helen Leite
January 28, 2026 AT 13:17EVERY SINGLE GENERIC IS MADE IN CHINA. THEY PUT SLEEPING DRUGS IN THEM SO YOU’LL BE QUIET. 🇨🇳💊 I saw a video. They inject the pills with microchips. That’s why they look different. It’s not the color. It’s the tracking. The FDA is in on it. Your doctor knows. They just don’t tell you. You think you’re saving money? You’re being watched.
STOP TAKING THE YELLOW PILLS.
Elizabeth Cannon
January 28, 2026 AT 14:41My aunt took a generic blood pressure med and her numbers went nuts. She had to go to the hospital. That’s not ‘bioequivalent.’ That’s a lie. I don’t care what the FDA says. If it doesn’t work for you, it doesn’t work. Period. And if your pharmacist tries to push it on you, say no. You’re not a lab rat. Pay the extra $10. Your life is worth more.
Also, why do they even make generics look so weird? Like… who designed these pills? A 5-year-old?
siva lingam
January 29, 2026 AT 22:54pharmacists care? really? they just want to move faster. patients care? nope. doctors care? lol. everyone just wants the pill to disappear and the bill to be low. the system is a joke. send help or more money. either one.