When people start using cannabis - whether for pain, anxiety, or sleep - they often don’t realize how deeply it can affect other medicines they’re taking. This isn’t just about feeling drowsy. It’s about cannabis drug interactions that can turn a safe treatment into a dangerous one. The science is clear: compounds in cannabis, especially CBD and THC, interfere with how your liver breaks down many common drugs. And that can mean the difference between healing and hospitalization.
How Cannabis Changes How Your Body Processes Medicines
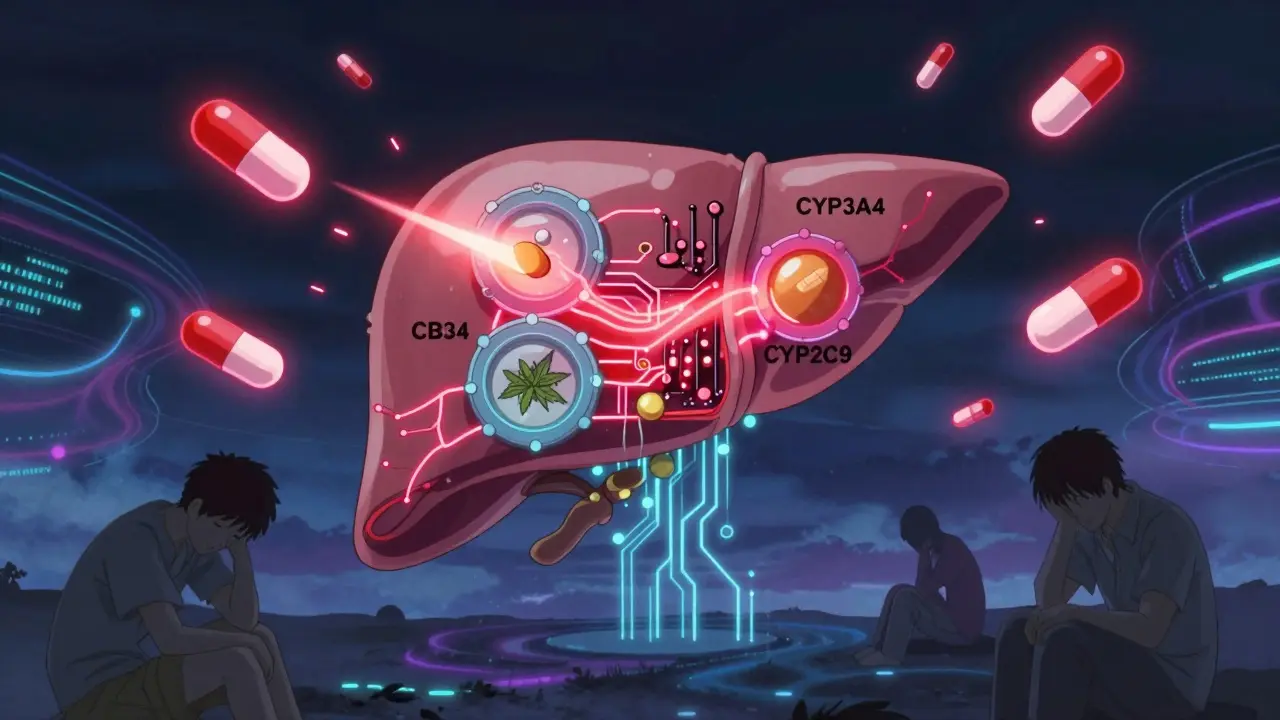
Your liver uses a group of enzymes called CYP450 to break down about 60% of all prescription drugs. Think of them as cleanup crews. CBD is a powerful inhibitor of two of these enzymes - CYP3A4 and CYP2C19. THC also shuts down CYP1A2, CYP2C9, and CYP3A4. When these enzymes slow down, your body can’t clear medications the way it should. That means drugs build up in your system. For some medications, even a small increase can cause serious side effects.
For example, if you’re taking clobazam for epilepsy, CBD can spike its levels by up to 500%. That’s not a little extra drowsiness - that’s confusion, weakness, and sometimes falling. A 2015 study found that nearly two-thirds of patients using CBD with clobazam needed their dose cut by 25% to 50%. And this isn’t rare. In a 2023 survey by the Epilepsy Foundation, 63% of CBD users reported increased sedation.
High-Risk Interactions: When Cannabis Can Be Life-Threatening
Some drug combinations with cannabis are not just risky - they’re dangerous. The biggest red flags involve medications with a narrow therapeutic index. That means the difference between the right dose and a toxic dose is tiny.
Warfarin, a blood thinner, is one of the most dangerous. Both CBD and THC block the enzyme that breaks it down (CYP2C9). One study tracking 17 cases found that within 72 hours of starting CBD, patients’ INR levels - a measure of blood clotting - jumped by 29% to 48%. That’s like going from a safe range to a bleeding risk zone. The American College of Clinical Pharmacy documented 12 cases of life-threatening bleeding in people using warfarin with cannabis. The American Society of Health-System Pharmacists now recommends checking INR every 3 to 5 days instead of weekly if cannabis is involved.
Tacrolimus, used by transplant patients to prevent organ rejection, is another high-risk drug. When taken with cannabis, its levels can surge 300% to 500% in just 72 hours. That can lead to kidney failure or nerve damage. In one documented case, a transplant patient on daily CBD needed to drop their tacrolimus dose by 60% to avoid toxicity.
Moderate-Risk Interactions: Watch for Subtle Changes
Not all interactions scream danger - but they still need attention. Benzodiazepines like alprazolam (Xanax) and opioids like oxycodone are common examples. Cannabis enhances their effects on the brain. Studies show this combination increases sedation by 35% to 60%. In older adults, that raises fall risk by 47%, according to the Pennsylvania Pharmacists Association.
Calcium channel blockers - such as amlodipine for high blood pressure - can also rise in concentration by 30% to 40% when mixed with cannabis. That leads to dizziness, fainting, or low blood pressure. One study found 15% to 25% of patients on amlodipine experienced these symptoms after starting CBD.
Even SSRIs like sertraline, often used for depression, can be affected. CBD raises sertraline levels by 10% to 15%. But unlike warfarin or tacrolimus, this rarely causes problems. Still, if you feel unusually tired or nauseous after adding CBD, it’s worth checking with your doctor.
What About Smoked Cannabis vs. Oils and Edibles?
The way you take cannabis changes the risk. Smoking delivers THC to your bloodstream in minutes. That means if you smoke and then take a sleeping pill or painkiller, the effects hit fast and hard. It’s easy to overdose on sedation.
Oral products like CBD oil or gummies take 2 to 4 hours to peak and last 6 to 8 hours. This creates a longer window for interactions. Warfarin, for example, stays in your system for days. If you take CBD oil every night, your INR might creep up slowly - and you might not notice until you start bruising easily.
Full-spectrum CBD products - which contain small amounts of THC - are more potent inhibitors than pure CBD isolates. Research shows they block CYP3A4 up to 37% more. So if you’re using a full-spectrum tincture, your risk is higher than if you’re using a THC-free product.
Real Stories, Real Risks
Online forums are full of firsthand accounts. One Reddit user, u/EpilepsyWarrior, wrote: “CBD increased my clobazam levels so much I couldn’t walk straight. My neurologist cut my dose by 40% immediately.” Another, u/ChronicPainSufferer, said they’d used 50mg of CBD daily with oxycodone for eight months with no issues.
That’s the problem - experiences vary wildly. Some people get sick. Others don’t. That’s why you can’t rely on anecdotes. A 2022 survey of 1,247 Reddit posts found that 38% of people using cannabis with benzodiazepines had to reduce their dose. But 41% of those on SSRIs noticed no change at all.
Even the form of cannabis matters. Smoking cannabis can actually speed up the breakdown of theophylline (used for asthma), lowering its levels by 25% to 30%. But cannabis tea? No effect on chemo drugs like docetaxel. The science is messy - and that’s why you need professional advice.

What Should You Do?
Don’t guess. Don’t assume. If you’re taking any prescription medication and considering cannabis, follow these steps:
- Be honest with your doctor. Tell them exactly what you’re using - product type, dose, and how often. Don’t say “I use CBD.” Say “I take 25mg of full-spectrum CBD oil every night.”
- Check your meds. High-risk drugs include warfarin, tacrolimus, clobazam, and some opioids. If you’re on one of these, don’t start cannabis without a plan.
- Get baseline tests. If you’re on warfarin, get your INR checked before starting. For tacrolimus, ask for a trough level. These numbers are your safety net.
- Monitor closely. Check for new side effects within 72 hours of starting or changing cannabis. Look for unusual bruising, dizziness, confusion, or extreme sleepiness.
- Space out your doses. Some experts suggest taking CBD at least 2 hours before or after other meds. It’s not proven, but it might help reduce overlap.
Pharmacists are your allies. Many now use tools like the University of Washington’s Cannabis Drug Interactions database. Ask yours to check your specific combo. If they say they don’t know - find one who does.
The Bigger Picture
More than 58 million Americans used cannabis in 2022. Over 40% of them were also on prescription drugs. Yet only 12 states require pharmacists to counsel patients on interactions. And 76% of community pharmacists say they feel unprepared to answer these questions.
The FDA has received over 1,300 reports of possible cannabis-medication reactions since 2018. That’s just the tip of the iceberg. Most people don’t report side effects. They just stop using one thing - or end up in the ER.
Research is catching up. A $2.3 million NIH-funded study at the University of Arkansas is tracking 200 patients on warfarin and CBD. Early data shows a 37% average INR rise at doses above 25mg/day. More studies are coming - but for now, caution is your best tool.
Final Thoughts
Cannabis isn’t inherently dangerous. But when it meets medications, it can become unpredictable. The same CBD that helps your seizures might push your blood thinner into dangerous territory. The same THC that eases your pain might make your sedative too strong.
There’s no one-size-fits-all answer. What works for one person can harm another. The only safe path is to talk to your care team - before you start. Don’t wait for a problem to happen. Ask now. Get tested. Adjust carefully. Your body will thank you.
Linda Franchock
February 15, 2026 AT 16:08Oliver Calvert
February 16, 2026 AT 01:46Agnes Miller
February 17, 2026 AT 03:48Digital Raju Yadav
February 17, 2026 AT 17:56PRITAM BIJAPUR
February 18, 2026 AT 21:12Geoff Forbes
February 19, 2026 AT 19:09Haley DeWitt
February 21, 2026 AT 08:14Brenda K. Wolfgram Moore
February 23, 2026 AT 05:49