When you take a blood thinner, you're trusting your body to stay balanced. These medications stop dangerous clots from forming-especially if you have atrial fibrillation, a replaced heart valve, or a history of deep vein thrombosis. But if too much builds up in your system, that same power becomes a threat: internal bleeding. And it doesn’t always look like a cut or a bruise. Sometimes, it starts quietly-dark stools, a persistent headache, urine that looks like tea. By the time you notice, it could already be life-threatening.
What Happens When a Blood Thinner Goes Too Far?
Blood thinners don’t make your blood "thin" like water. They interfere with the proteins your body uses to form clots. Warfarin, the oldest and still widely used drug, blocks vitamin K, which your liver needs to make clotting factors. Newer ones-like apixaban (Eliquis), rivaroxaban (Xarelto), and dabigatran (Pradaxa)-target different parts of the clotting process. All of them work well. But if you take too much, or if your body can’t clear it properly, your blood loses its ability to seal even tiny breaks in vessels.The danger isn’t just bleeding from a cut. It’s internal. Bleeding inside your skull, gut, kidneys, or muscles can go unnoticed for hours. That’s why symptoms often sneak up. You might feel tired, dizzy, or just "off." Your stool turns black and tarry. Your urine looks pink or brown. You vomit something that looks like coffee grounds. These aren’t just inconvenient-they’re red flags.
For warfarin users, doctors track a number called INR. A normal INR is around 1.0. For most people on warfarin, the target is 2.0 to 3.0. If your INR climbs above 4.5, you’re in danger zone. Above 7.0? That’s a medical emergency. One study found that patients with INR over 10 had a 28% chance of major bleeding within 30 days-even if they felt fine.
Signs You’re Bleeding Inside (Don’t Wait for a Hemorrhage)
Many people delay going to the hospital because they think, "It’s probably nothing." But here’s what you need to know: if you’re on a blood thinner and you notice any of these, call emergency services right away.- Black, sticky, or bloody stools
- Pink, red, or dark brown urine
- Vomiting blood or material that looks like coffee grounds
- Unexplained bruising, especially large patches or spots that appear without injury
- Small red or purple dots under the skin (petechiae)
- Nosebleeds or gum bleeding that lasts longer than 10 minutes
- Heavy menstrual bleeding (soaking through a pad in under an hour)
- Severe headache, confusion, vision changes, or dizziness (could mean brain bleeding)
- Sharp pain in the abdomen, lower back, or chest
- Weakness, fainting, or sudden difficulty breathing
A 2022 survey by the National Blood Clot Alliance found that 62% of patients ignored early symptoms for more than 12 hours. One Reddit user, u/WarfarinWarrior, wrote: "I thought my dark stools were from eating beets. By the time I got to the ER, my hemoglobin was 6.2. I needed three units of blood."
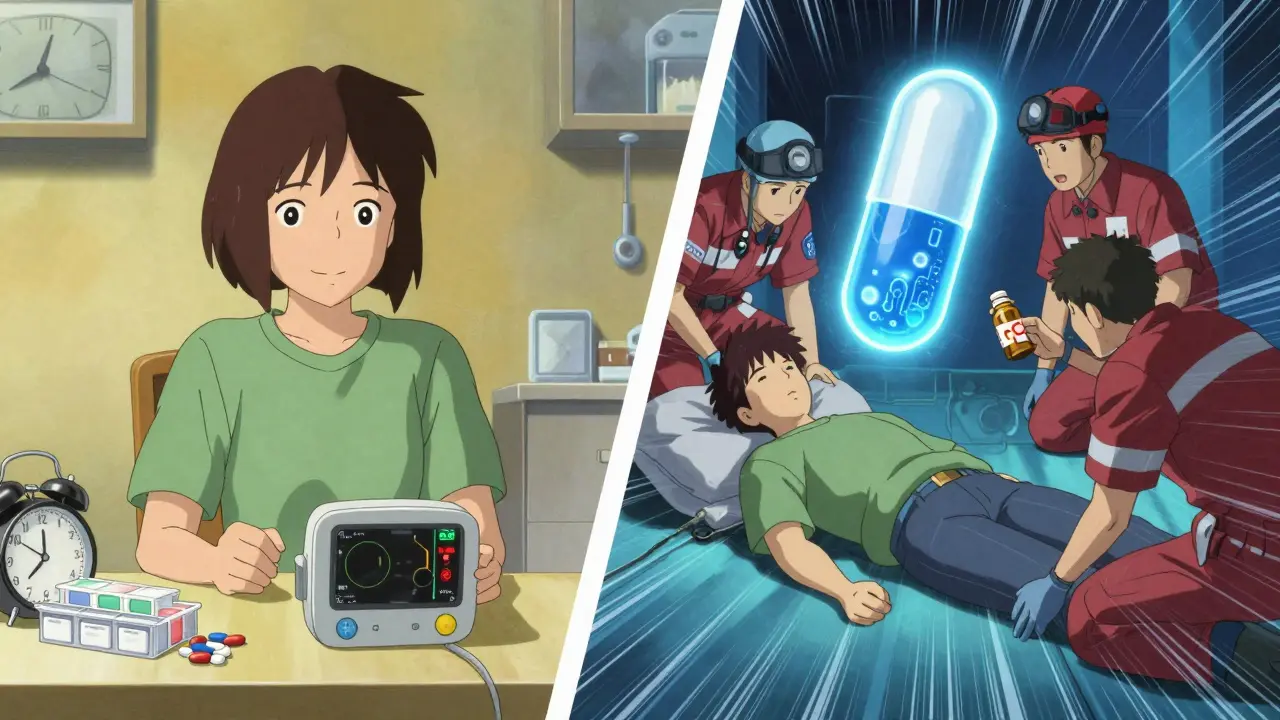
What to Do Right Now-Step by Step
If you suspect an overdose or internal bleeding, time is everything. Don’t wait to see if it gets worse. Don’t call your doctor and wait for an appointment. Go straight to emergency care.- Call emergency services immediately. In Australia, dial 000. Say: "I’m on a blood thinner and I think I’m bleeding internally." This gets you priority response.
- Do not take another dose. Even if you think you missed one, don’t double up. More won’t fix it-it will make it worse.
- Write down what you took. Name of the drug, dose, and time of last intake. If you have the pill bottle, bring it.
- Don’t take NSAIDs. No aspirin, ibuprofen, naproxen, or other painkillers. These make bleeding worse.
- Lie down and elevate bleeding areas. If you’re bleeding externally (nose, cut), apply firm pressure for at least 10 minutes. Don’t peek. Keep pressure steady.
- Stay calm. Panic raises your heart rate and blood pressure, which can speed up bleeding. Breathe slowly.
For patients on warfarin, emergency teams will check your INR right away. If it’s dangerously high, they’ll give you vitamin K orally or intravenously. For severe cases, they’ll use 4-factor Prothrombin Complex Concentrate (PCC)-a fast-acting clotting agent that can reverse warfarin’s effect in minutes.
For newer drugs like Eliquis or Xarelto, reversal agents exist. Andexanet alfa reverses factor Xa inhibitors. Idarucizumab reverses Pradaxa. These aren’t magic pills-they cost thousands of dollars and aren’t always available. But they work. And they’re why timing matters.

What Hospitals Will Do
Emergency teams don’t guess. They test. They look for signs of bleeding in your brain, belly, and kidneys. They’ll do a CT scan if you have head trauma or a severe headache. They’ll check your hemoglobin-if it’s dropped below 8 g/dL, you’re likely losing blood internally.If you’re stable but have a high INR with no bleeding, you might get oral vitamin K and be sent home with close follow-up. But if you’re bleeding? You’re going straight to the ICU. They’ll give you PCC or FFP (fresh frozen plasma), vitamin K, and possibly tranexamic acid-a drug that helps stop bleeding by stabilizing clots.
One 2023 study showed that patients who received PCC within 90 minutes of symptom onset had 94% survival rates. Those who waited over four hours? Survival dropped to 59%.
Prevention Is the Best Medicine
The best way to avoid an overdose? Stay in control.- Use a pill organizer with clear labels.
- Set phone alarms for doses and INR checks.
- Never change your dose without talking to your doctor.
- Keep a list of all medications-especially antibiotics, supplements, or herbal products. Many interact with blood thinners.
- Get your INR checked regularly. If you’re on warfarin, weekly checks are common at first. Once stable, monthly is fine. But if your INR keeps jumping up and down, you need more frequent testing.
- Use a bleeding risk checklist. The HAS-BLED score (Hypertension, Abnormal kidney/liver, Stroke, Bleeding history, Labile INR, Elderly, Drugs/alcohol) helps doctors decide if you’re high risk. If you score 3 or more, you need extra monitoring.
Some patients now use home INR monitors. These small devices cost around $250 and let you test your blood at home. Studies show they reduce major bleeding events by 34%. If your doctor says you’re at high risk, ask if you’re eligible for one.
What You Should Know About the New Reversal Drugs
The future of anticoagulant overdose is changing. Ciraparantag, a new universal reversal agent, is in final trials. It works on all types of blood thinners-warfarin, heparin, and DOACs. If approved, it could cut reversal time from hours to minutes. That’s huge. But it’s not here yet.Right now, the best tools are still vitamin K, PCC, and knowing your body. Don’t rely on future breakthroughs. Use what’s available now.
Why This Matters More Than You Think
Blood thinners are among the most common medications in Australia. In 2023, over 180,000 Australians were on warfarin alone. The cost of a major bleeding episode? Around $28,000 in hospital bills. Many patients lose work, need long-term care, or suffer permanent damage.But here’s the truth: most of these emergencies are preventable. You don’t need to be a medical expert. You just need to know the signs. You need to act fast. And you need to tell someone-anyone-if you’re feeling wrong.
What should I do if I think I took too much of my blood thinner but I feel fine?
Even if you feel fine, a blood thinner overdose can cause delayed bleeding. Call your doctor or go to the emergency department immediately. Your INR may be dangerously high, and internal bleeding can start without symptoms. Don’t wait for bruising or pain. Get tested.
Can I reverse a blood thinner overdose at home?
No. Vitamin K or other treatments require medical supervision. Taking extra vitamin K on your own won’t help and could cause dangerous side effects. Emergency treatment with PCC, IV fluids, or reversal agents must be given in a hospital. Home remedies won’t work and may delay life-saving care.
Do all blood thinners have reversal agents?
No. Warfarin can be reversed with vitamin K and PCC. Dabigatran (Pradaxa) has idarucizumab. Apixaban and rivaroxaban (Xarelto) can be reversed with andexanet alfa. But there’s no approved reversal agent for all types. That’s why knowing which drug you’re on-and acting fast-is critical.
Can I take painkillers if I’m on a blood thinner and I have a headache?
Avoid aspirin, ibuprofen, naproxen, and other NSAIDs. They increase bleeding risk. Use acetaminophen (paracetamol) instead, but only if approved by your doctor. If your headache is severe or sudden, don’t take anything-go to the hospital. It could be a brain bleed.
How often should I get my INR checked?
When you first start warfarin, you may need weekly checks. Once your dose is stable and your INR stays in range, monthly testing is usually enough. But if your INR fluctuates, if you start new medications, or if you change your diet (especially vitamin K-rich foods like kale or spinach), you may need testing every few days. Always follow your doctor’s schedule.
What should I do if I miss a dose of my blood thinner?
If you miss a dose, don’t double up the next day. Call your doctor or pharmacist for advice. Missing one dose usually won’t cause clots, but doubling up can lead to overdose. Keep a log of missed doses and bring it to your next appointment.
Can alcohol affect my blood thinner?
Yes. Alcohol can increase the risk of bleeding and interfere with how your liver processes warfarin. Occasional light drinking (one drink a day) is usually okay, but binge drinking or daily heavy use can cause dangerous INR spikes. Always talk to your doctor about your alcohol use.
Are there foods I should avoid while on blood thinners?
For warfarin users, consistency matters more than avoidance. Vitamin K, found in leafy greens like spinach, kale, and broccoli, affects how warfarin works. Don’t stop eating them-but don’t suddenly eat a lot more or less than usual. Keep your intake steady. For DOACs like Eliquis or Xarelto, diet has less impact, but grapefruit and St. John’s Wort can interfere with some drugs. Always check with your pharmacist.
Next Steps: Protect Yourself Before It’s Too Late
If you’re on a blood thinner, here’s what to do today:- Check your pill bottle. Do you know the exact name and dose?
- Call your doctor. Ask: "What’s my target INR? When’s my next test?"
- Write down the signs of internal bleeding. Tape them to your fridge.
- Give a copy of your medication list to a family member or friend.
- Set a weekly phone reminder: "Check INR date. Call doctor if I feel off."
You don’t need to live in fear. But you do need to be ready. Because when it comes to blood thinners, knowing the signs-and acting fast-can save your life.

John Sonnenberg
February 8, 2026 AT 07:58Joshua Smith
February 9, 2026 AT 15:56Elan Ricarte
February 11, 2026 AT 14:03Camille Hall
February 12, 2026 AT 07:09Jonah Mann
February 14, 2026 AT 00:02THANGAVEL PARASAKTHI
February 14, 2026 AT 22:33Frank Baumann
February 16, 2026 AT 19:52Chelsea Deflyss
February 18, 2026 AT 09:44Scott Conner
February 19, 2026 AT 13:28