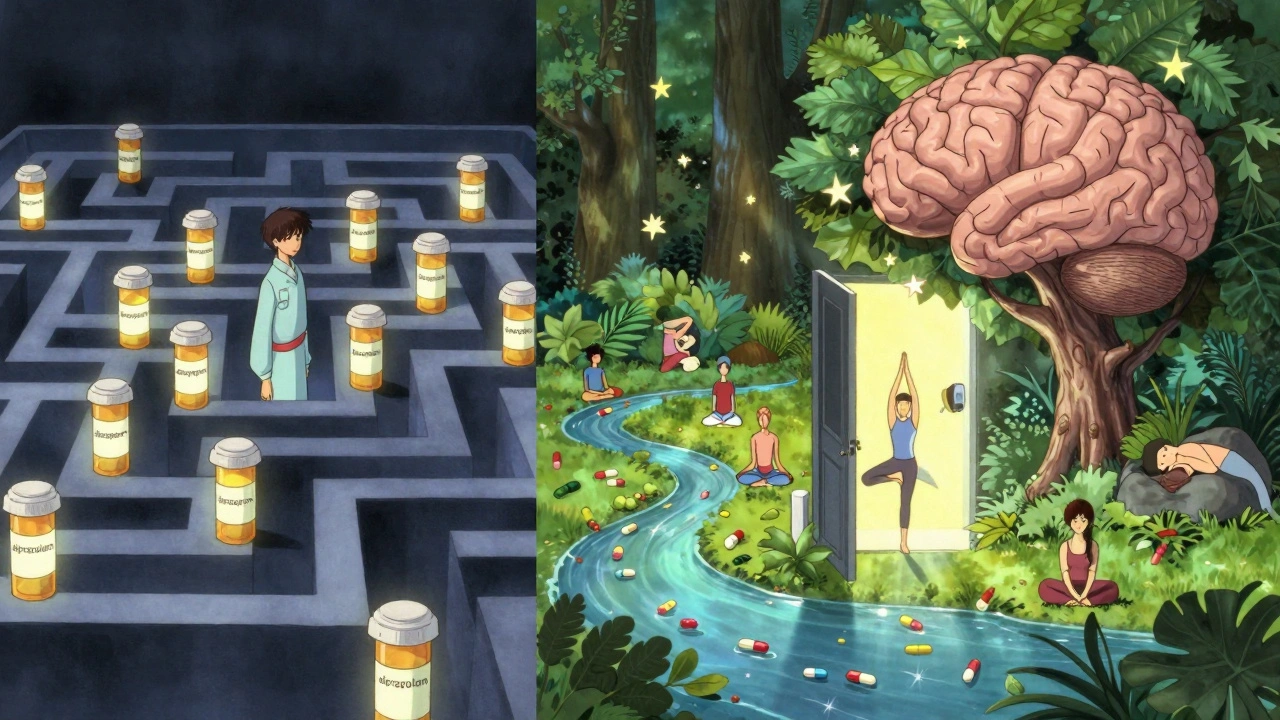
For decades, benzodiazepines have been one of the most common prescriptions for sudden anxiety, panic attacks, and sleep problems. They work fast - often within an hour - and can turn a crushing panic episode into something manageable. But for every person who says they saved their life, another talks about being trapped in a cycle they couldn’t escape. The truth isn’t black and white. Benzodiazepines are powerful tools, but they come with serious trade-offs that most people don’t fully understand until it’s too late.
How Benzodiazepines Work
Benzodiazepines don’t just make you feel calm - they change how your brain processes fear. They boost the effect of GABA, a natural chemical that slows down overactive nerve signals. Think of your brain as a room full of people yelling. GABA is the person who says, ‘Hey, lower your voices.’ Benzodiazepines hand that person a megaphone. That’s why they work so quickly for panic attacks, seizures, or extreme muscle spasms. Drugs like alprazolam (a short-acting benzodiazepine used for panic disorder and anxiety), diazepam (a long-acting option used for anxiety, muscle spasms, seizures, and alcohol withdrawal), and lorazepam (often used in hospitals for acute agitation or seizure control) are all built on this same mechanism.
But speed comes at a cost. Because they act so directly on brain circuits, your brain starts to rely on them. After just a few weeks, your natural GABA system begins to downsize. You don’t need as much of your own calming chemical anymore because the drug is doing it for you. That’s the first step toward dependence - and it happens faster than most people expect.
When Benzodiazepines Help
There are real, life-saving uses for these drugs. In emergency rooms, midazolam (a fast-acting benzodiazepine used for status epilepticus and procedural sedation) stops seizures when nothing else works. For someone having a panic attack on a plane or during a medical procedure, a single dose of alprazolam can restore control. In alcohol withdrawal, chlordiazepoxide (a long-acting benzodiazepine used to prevent delirium tremens) prevents dangerous spikes in brain activity that can lead to seizures or death.
For short-term use - think a few days to a couple of weeks - they’re unmatched. A 2023 study in JAMA Internal Medicine found that patients who used benzodiazepines for just 10 days while also doing cognitive behavioral therapy had a 58% lower chance of becoming dependent than those who took the drug alone. That’s the sweet spot: fast relief, paired with a plan to get off it.
Doctors still prescribe them for this reason. The American Psychiatric Association says it’s okay - even recommended - for acute anxiety if used for 2 to 4 weeks max. The problem isn’t the drug. It’s what happens when the timeline gets stretched.
The Hidden Risk: Dependence
Here’s what most people don’t realize: if you take benzodiazepines every day for more than four weeks, your body will physically change. About 30 to 50% of patients develop dependence, according to the World Health Organization. That doesn’t mean you’re addicted. It means your brain now needs the drug to function normally. Stop it suddenly, and your nervous system goes into overdrive.
Withdrawal isn’t just feeling anxious again. It can mean:
- Severe rebound anxiety, worse than before you started
- Insomnia so bad you can’t sleep for days
- Tremors, sweating, heart palpitations
- Seizures in extreme cases
- Feeling like you’re detached from reality - derealization or depersonalization
Reddit threads from r/Anxiety and r/PharmaCon are full of stories from people who took a prescription for a month, then couldn’t quit. One user wrote: ‘I tapered for 8 months. I still wake up with panic at 3 a.m.’ Another said: ‘I didn’t know I was dependent until I tried to stop. My hands shook so hard I couldn’t hold a coffee cup.’
And it’s not just emotional. Benzodiazepines cause anterograde amnesia (a condition where new memories aren’t formed). Around 23% of users in a 2022 survey reported memory gaps during daily tasks - forgetting conversations, losing keys, missing appointments. That’s not just inconvenient. It’s dangerous.

Who’s Most at Risk?
Not everyone who takes benzodiazepines ends up dependent. But certain factors make it more likely:
- Taking them daily for longer than 4 weeks
- Using higher doses than prescribed
- Having a history of substance use or mental health disorders
- Being over 65 - older adults are 50% more likely to fall and 32% more likely to develop dementia with long-term use, according to the American Geriatrics Society 2023 Beers Criteria
- Using them with alcohol or opioids - a deadly combo that increases overdose risk
Women are prescribed benzodiazepines more often than men - 8.3 prescriptions per 100 women versus 4.3 per 100 men in the U.S. in 2021. Why? Often because they’re more likely to be diagnosed with anxiety and less likely to be offered therapy first. That’s not bias - it’s a gap in care.
Alternatives That Work Better Long-Term
Antidepressants like SSRIs and SNRIs take 4 to 6 weeks to kick in, but once they do, they’re safer for ongoing use. They don’t cause dependence, drowsiness, or memory loss. For chronic anxiety, they’re the gold standard.
For insomnia, Cognitive Behavioral Therapy for Insomnia (CBT-I) (a structured, non-drug treatment that reprograms sleep habits) has been proven to work better than any sleep medication - even long-term. Studies show people who complete CBT-I stay asleep for years. Benzodiazepines? Effects fade after 2 to 4 weeks.
For panic attacks, exposure therapy helps you face triggers without running. For muscle spasms, physical therapy and stretching often work better than muscle relaxants. And for alcohol withdrawal, medical detox with supervision and non-benzodiazepine medications like baclofen or gabapentin are gaining traction.
The bottom line: benzodiazepines are emergency tools. Not maintenance tools.
What Safe Use Looks Like
If you’re prescribed a benzodiazepine, here’s how to use it safely:
- Ask your doctor: ‘Is this for short-term use only?’
- Set a clear end date - no more than 2 to 4 weeks.
- Never increase the dose without talking to your doctor.
- Avoid alcohol completely while taking it.
- Keep a journal: note your mood, sleep, and any side effects.
- Plan your exit before you start. Ask about a tapering schedule.
If you’ve been on them longer than recommended, don’t quit cold turkey. That’s when seizures and extreme withdrawal happen. The Ashton Manual (the gold standard guide for benzodiazepine tapering) recommends reducing your dose by 5-10% every 1 to 2 weeks. For someone on a high dose for years, that can take 6 months to over a year. It’s slow, but it works.
Many hospitals and clinics now use electronic alerts to flag prescriptions longer than 90 days. Kaiser Permanente cut long-term benzodiazepine use by 37% just by adding that one system. You don’t have to be alone in this.
The Future of Benzodiazepines
The FDA added a boxed warning in 2020 - the strongest possible - about abuse, dependence, and withdrawal. Countries like the UK and Canada now recommend against starting benzodiazepines for anxiety at all. The U.S. still prescribes them, but rates are falling. In 2021, 76 million prescriptions were filled. By 2027, Evaluate Pharma predicts a 15-20% drop as doctors shift to safer alternatives.
They’re not going away. Not yet. For someone in status epilepticus, or in the middle of a life-threatening panic attack, they’re still the fastest, most reliable option. But their role is shrinking. The future belongs to therapies that heal, not just numb.
Can benzodiazepines cause memory loss even at normal doses?
Yes. Even at prescribed doses, benzodiazepines can cause anterograde amnesia - where your brain stops forming new memories during the time the drug is active. About 23% of users in a 2022 survey reported gaps in memory, like forgetting conversations or misplacing items. This is a known side effect, not a rare accident.
How long does it take to get addicted to benzodiazepines?
Physical dependence can develop in as little as 2 to 4 weeks with daily use. Addiction - which includes compulsive use despite harm - takes longer and varies by person. But dependence, the body’s adaptation to the drug, happens quickly. That’s why doctors are told to limit prescriptions to short-term use.
Are there safer alternatives to benzodiazepines for anxiety?
Yes. For long-term anxiety, SSRIs and SNRIs are more effective and don’t cause dependence. For panic attacks, cognitive behavioral therapy (CBT) is proven to work as well or better than medication. For insomnia, CBT-I is the first-line treatment and has lasting results. Non-benzodiazepine sleep aids like zolpidem carry their own risks but are less likely to cause dependence than benzodiazepines.
Can you die from benzodiazepine withdrawal?
Yes, in rare cases. Sudden withdrawal after long-term use can trigger seizures, delirium, or cardiovascular collapse. That’s why tapering under medical supervision is critical. Never stop cold turkey. The Ashton Manual provides safe, step-by-step guidelines for reducing doses gradually over months.
Why are benzodiazepines still prescribed if they’re so risky?
Because they work - quickly and effectively - for acute situations. For someone having a seizure, a panic attack in an ER, or severe alcohol withdrawal, benzodiazepines are life-saving. The issue isn’t their use in emergencies. It’s their overuse for chronic conditions like generalized anxiety, where safer, long-term options exist.
Is it possible to get off benzodiazepines after long-term use?
Yes, but it takes time and support. Most people need 3 to 6 months, sometimes longer, to taper safely. Success rates are high with medical supervision and behavioral therapy. Many people report feeling clearer, calmer, and more in control after quitting - even if the process was hard. You’re not broken if you need help getting off. You’re human.
What to Do Next
If you’re currently taking benzodiazepines and have been for more than a month, talk to your doctor about a tapering plan. Don’t wait until you feel stuck. If you’re struggling with withdrawal, find a specialist in addiction medicine or a clinic that follows the Ashton Manual. Support groups like Benzodiazepine Support Group or online communities can help you feel less alone.
If you’ve never taken them but are considering it for anxiety or sleep - ask about therapy first. CBT, mindfulness, and sleep hygiene are powerful, lasting tools. Medication should be a bridge, not a permanent solution.
Benzodiazepines aren’t evil. They’re tools - sharp, fast, and dangerous if misused. Use them wisely, and they can help. Use them carelessly, and they can take years of your life.

Roger Leiton
December 3, 2025 AT 13:27ATUL BHARDWAJ
December 4, 2025 AT 10:59Steve World Shopping
December 6, 2025 AT 03:26Rebecca M.
December 7, 2025 AT 01:13Shannara Jenkins
December 8, 2025 AT 23:40Elizabeth Grace
December 9, 2025 AT 05:32Steve Enck
December 10, 2025 AT 15:56Jay Everett
December 11, 2025 AT 20:01मनोज कुमार
December 13, 2025 AT 13:52Joel Deang
December 14, 2025 AT 15:00Arun kumar
December 16, 2025 AT 14:36Zed theMartian
December 17, 2025 AT 15:13Alicia Marks
December 19, 2025 AT 04:44Paul Keller
December 20, 2025 AT 02:10