The Pharmaceutical Benefits Scheme (PBS) is the backbone of Australia’s healthcare system when it comes to prescription drugs. It’s not just a subsidy program-it’s what keeps millions of Australians from choosing between medicine and groceries. Since 1948, the PBS has ensured that essential drugs are affordable, no matter your income. But behind the scenes, it’s a complex machine shaped by politics, economics, and real human struggles. And at the heart of it all? Generic medicines.
How the PBS Works-Simply Put
The PBS doesn’t give you free medicine. It cuts the price. If a drug costs $100, the government pays most of it. You pay a co-payment. As of January 1, 2026, that’s $25 for most people and just $7.70 for concession card holders. That’s a big drop from the $31.60 it was just months ago. The government sets these prices based on what’s fair, what’s effective, and what the country can afford. Every medicine on the PBS has to pass a strict review by the Pharmaceutical Benefits Advisory Committee (PBAC). They don’t just look at whether a drug works-they ask: Is it worth the cost? Their benchmark? Around $50,000 per quality-adjusted life year (QALY). That means if a drug extends someone’s life by a year with good quality, and it costs less than $50,000 per year gained, it’s usually approved. But there are exceptions. For rare diseases, the PBAC will go higher-sometimes over $150,000 per QALY. There are three types of PBS listings:- General benefits: Available to anyone with a Medicare card.
- Restricted benefits: Only for specific conditions-like a diabetes drug that can’t be used for prediabetes.
- Authority required: You need special approval before you can get it. This is where things get messy.
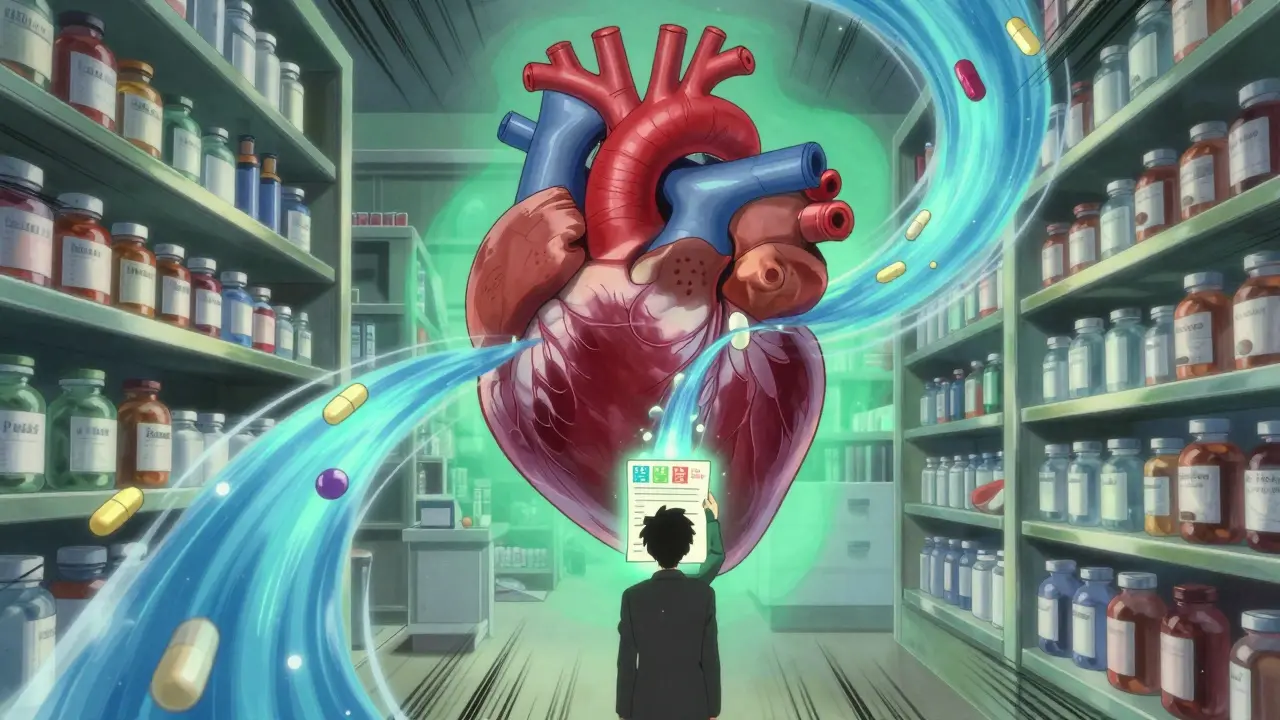
Why Generics Dominate the PBS
Australia’s generic drug market is massive. In 2024, generics made up 84% of all prescriptions dispensed under the PBS by volume. That’s higher than the OECD average. But here’s the twist: they only account for 22% of total PBS spending. Why? Because originator drugs-brand-name medicines-are still expensive, even after patents expire. The PBS uses something called reference pricing. If five drugs treat the same condition, the government picks the cheapest one as the benchmark. All others get priced relative to it. So if a generic hits the market at half the price of the brand, the brand’s subsidy drops too. That forces companies to compete on price. The rules are strict. After six months, a generic’s reference price is set at 60% of the original drug. After a year, it drops to 43%. That’s why prices crash. In cardiovascular drugs, the average generic price falls by 74% within a year of multiple generics entering the market. Statins? By 18 months after patent expiry, 95% of prescriptions are for generics. The top five generic manufacturers-Symbion, Sigma, Mylan, Aspen, and Hospira-control nearly 70% of the market. They’re not just filling prescriptions; they’re reshaping Australia’s healthcare spending.Who Pays? And Who Struggles?
It’s easy to think everyone benefits equally. But that’s not true. Concession card holders-pensioners, disability recipients, low-income families-pay $7.70 per script. They can get 60-day prescriptions for the same price as a 30-day one. That’s a 50% saving. For many, it’s the difference between taking their meds or not. But general patients? They pay $25. That might sound reasonable until you add up five medications. $125 a month. $1,500 a year. And that’s before the safety net. The PBS safety net kicks in after you’ve spent $1,571.70 in a calendar year. After that, your co-payment drops to $7.70-even if you’re not a concession holder. That’s lifesaving for people with chronic illnesses. But hitting that threshold takes time. Many don’t make it. The Australian Bureau of Statistics found that 12.3% of general patients skip doses or don’t fill prescriptions because of cost. That’s 1.8 million people. On Reddit, users share stories like: “I’m a retiree. My five meds cost $158 a month. I cut back on food.” The Australian Council of Social Service says 28% of low-income households with multiple chronic conditions reduce food spending to afford medicine.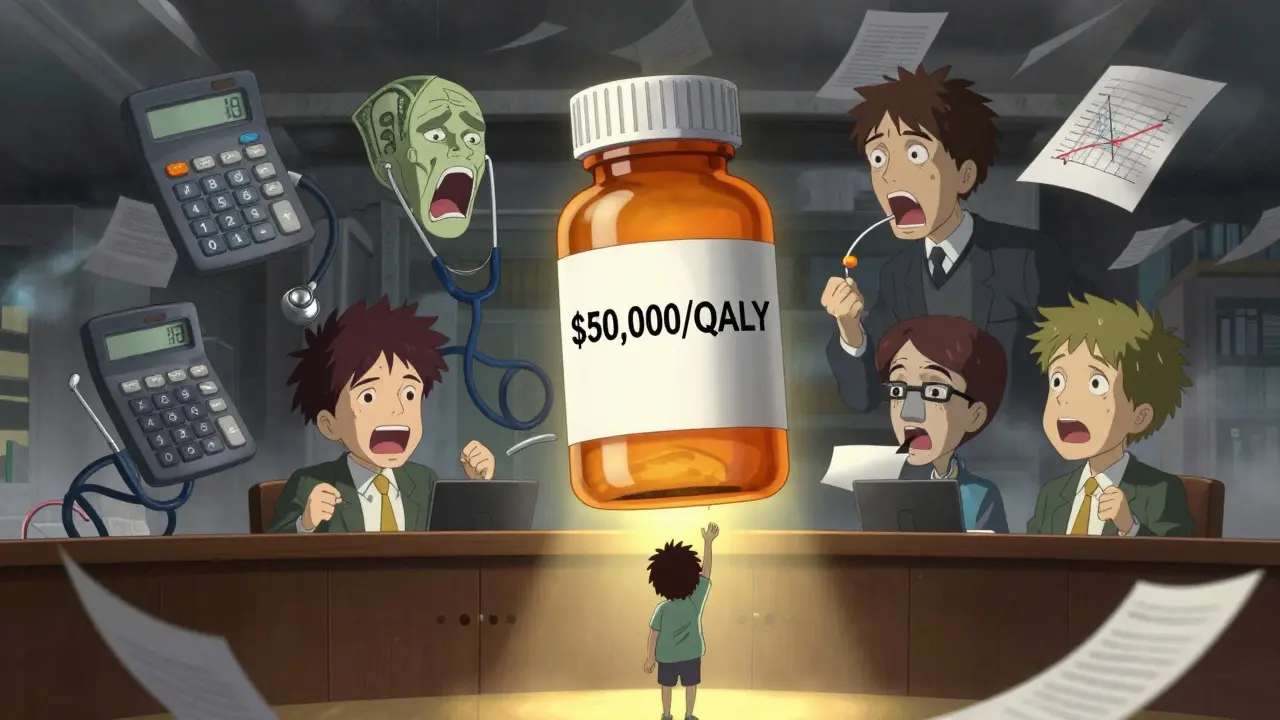
The Delays That Hurt Patients
Here’s the ugly truth: just because a drug is approved in Australia doesn’t mean it’s on the PBS. The Therapeutic Goods Administration (TGA) approves new medicines for safety. But getting them onto the PBS? That’s a whole other process. On average, it takes 14.2 months from TGA approval to PBS listing. During that time, patients pay full price-often $1,850 or more out of pocket. KPMG found the median time from global launch to PBS listing is 587 days. In Germany? 320 days. In Canada? 410. That’s a gap. And it’s not just about money. It’s about lives. A cancer patient might wait over a year for a life-extending drug because the PBAC hasn’t reviewed it yet. The Highly Specialised Drugs Program (HSDP) was created for rare diseases. But it has eight strict criteria. Many drugs fail because they don’t meet all of them-even if they help. In 2025, reforms began to loosen two of those criteria. Progress, but slow.What’s Changing in 2026 and Beyond
The government isn’t sitting still. The National Health Amendment (Cheaper Medicines) Bill 2025, passed in May 2025, cut the general co-payment from $31.60 to $25.00 starting January 1, 2026. That’s a $784.6 million saving for patients over four years. But it means the government will spend $689 million more. Budget 2025-26 added $1.2 billion for new PBS listings. Drugs like Talazoparib for prostate cancer and Relugolix for endometriosis are now covered. That’s 150,000 more Australians getting access. The Department of Health is also pushing digital changes. Real-time prescription monitoring, AI-driven reviews of prescribing patterns, and faster electronic authority approvals are all in motion. Right now, paper-based authority requests take over 7 days to process. Electronic ones take under 2. That’s a big deal for pharmacists and patients alike. But challenges remain. The Productivity Commission found delays in generic substitution after patent expiry average 217 days. That’s seven months of patients paying full price when cheaper alternatives exist.
Global Comparisons-Where Australia Stands
Compared to the U.S., Australia’s system is a steal. Generic drugs cost 30-40% less than in the U.S. But compared to the UK? They’re 15-20% more expensive. The UK’s NHS has a tighter price control system. The UK’s NICE uses a hard cap of £20,000-£30,000 per QALY. Australia’s PBAC is more flexible. That’s why some ultra-expensive drugs get listed here but not there. But that flexibility comes at a cost-longer wait times. The PBS is praised for its efficiency. The Grattan Institute says it saves Australian households $13 billion a year in out-of-pocket costs. But critics warn: without reform, PBS spending could hit 2.6% of GDP by 2045. In 2005, it was 0.7%. That’s unsustainable.What This Means for You
If you’re on a concession card: you’re covered well. Use the 60-day script trick. It saves you money without extra hassle. If you’re a general patient: track your PBS spending. Once you hit the safety net, your costs drop dramatically. Use the Services Australia PBS app to monitor your spending in real time. If you’re prescribed a new medicine: check if it’s on the PBS. If it’s not, ask your doctor about alternatives. Sometimes, there’s a cheaper, PBS-listed drug that works just as well. If you’re a prescriber: learn the PBS rules. Authority-required listings are a nightmare. Use the online tools. Submit electronically. It saves time for you and your patients. The PBS isn’t perfect. But it’s one of the most effective public health programs in the world. It keeps people alive. It keeps families from going broke. And it’s built on the power of generics. The real story isn’t just about prices. It’s about access. It’s about fairness. And it’s about whether we’re willing to keep fixing the system before it breaks.What is the PBS and how does it work?
The Pharmaceutical Benefits Scheme (PBS) is Australia’s government program that subsidizes the cost of prescription medicines. It makes essential drugs affordable by covering most of the price. Patients pay a co-payment-$25 for general patients and $7.70 for concession card holders as of January 2026. The government negotiates prices with drug companies and lists medicines based on clinical need and cost-effectiveness.
How do generic medicines affect PBS costs?
Generics drive down PBS spending. Once a brand-name drug’s patent expires, generic versions enter the market. The PBS uses reference pricing, setting the subsidy based on the cheapest option. This forces prices down-sometimes by over 70% within a year. Generics make up 84% of prescriptions by volume but only 22% of total PBS spending because brand-name drugs remain expensive even after generics arrive.
Why are some medicines not available on the PBS?
A medicine must pass review by the Pharmaceutical Benefits Advisory Committee (PBAC), which assesses clinical effectiveness and cost-effectiveness. Many drugs are too expensive per quality-adjusted life year (QALY), or the manufacturer hasn’t applied for listing. Even after TGA approval, it can take over a year for a drug to be added to the PBS, leaving patients to pay full price.
What is the PBS safety net and how does it help?
The PBS safety net is a cap on out-of-pocket costs. Once you’ve spent $1,571.70 on PBS medicines in a calendar year, your co-payment drops to $7.70 per script-no matter if you’re a general or concession patient. This protects people with chronic conditions who need multiple medications. Many rely on it to avoid choosing between medicine and essentials like food.
How can I check if my medicine is on the PBS?
You can check the PBS website (updated monthly), use the Services Australia PBS app (downloaded over 1.2 million times), or call the PBS helpline at 1800 020 299. Your pharmacist can also confirm whether your medicine is subsidized. Always ask if there’s a cheaper, PBS-listed alternative.
What’s the difference between a concession card and general patient co-payment?
Concession card holders (pensioners, disability recipients, low-income families) pay $7.70 per PBS script. General patients pay $25.00 as of January 2026. Concession holders can also get 60-day prescriptions for the same price as a 30-day one, saving 50%. The safety net ensures that once general patients spend $1,571.70 in a year, their co-payment also drops to $7.70.
Why do some medicines take so long to get on the PBS?
After the Therapeutic Goods Administration (TGA) approves a drug, the manufacturer must apply for PBS listing. The Pharmaceutical Benefits Advisory Committee (PBAC) then reviews it for cost-effectiveness, which can take months. The average time from TGA approval to PBS listing is 14.2 months. This delay forces patients to pay full price-often over $1,800-for life-saving drugs.
Ian Long
January 10, 2026 AT 05:40Man, I didn't realize generics were that dominant in Australia. 84% of prescriptions but only 22% of spending? That's wild. The reference pricing system sounds like a genius hack to keep prices down. I wish the US could pull something like this off without pharmaceutical companies throwing tantrums.
Pooja Kumari
January 12, 2026 AT 00:16So let me get this straight - the government sets a price ceiling based on some fancy math called QALY and then forces companies to compete? That’s so... logical. In India, we just pay whatever the pharmacy says, and if you can’t afford it, you pray. I’m kinda jealous. Also, I just looked up my dad’s blood pressure med - it’s on PBS? Wow. I’m crying. Not because I’m emotional, but because I just realized how lucky Australians are. Also, I’m sending this to my cousin in Mumbai. She needs to see this.
Jacob Paterson
January 14, 2026 AT 00:00Oh wow, Australia’s got a socialist drug program? How quaint. Next they’ll start giving out free yoga and kombucha. The fact that you’re proud of paying $25 for meds instead of $150 is pathetic. You’re not saving money - you’re just being exploited by a bureaucracy that thinks it knows better than the market. Also, 14 months to list a drug? That’s not a system. That’s a funeral.
Angela Stanton
January 15, 2026 AT 15:19Let’s unpack the QALY metric - it’s essentially a utilitarian calculus where life = $50k. But here’s the kicker: PBAC’s flexibility for rare diseases (up to $150k/QALY) creates a two-tiered system where the ultra-rare get subsidized while common chronic conditions? Still stuck at $25/co-pay. And don’t get me started on the 217-day generic delay. That’s not inefficiency - that’s predatory inertia. Pharma’s playing 4D chess while patients are stuck in checkers. 🤷♀️
Jerian Lewis
January 17, 2026 AT 08:21People act like $25 is nothing. But if you’re on disability and need 5 meds? That’s $125 a month. That’s a rent payment. That’s groceries gone. The safety net is a joke - you have to spend over $1,500 first. That’s not help. That’s a trap.
Kiruthiga Udayakumar
January 17, 2026 AT 08:43My cousin in Sydney just told me her mom got her diabetes meds for $7.70 - she cried. I told her, 'That’s what socialism looks like, beta.' 😭 We don’t even have a basic health card in India. You pay or you don’t eat. I’m so mad I could scream. But also… kinda proud of Australia? Not for the government, but for the people who fought for this. You guys didn’t just accept it. You demanded it.
Patty Walters
January 19, 2026 AT 03:02Just a heads up - if you're on the safety net, make sure you're tracking your spending. I missed it for 8 months because I didn't realize the app auto-syncs with your Medicare account. Once I turned it on, my co-pay dropped to $7.70 and I almost did a happy dance. Also, don't forget to ask your pharmacist about generic alternatives - they know way more than your doctor sometimes. 💊
Maggie Noe
January 19, 2026 AT 11:53It’s funny how we treat medicine like a commodity. We say 'it's worth $50k per year of life' like that's a number you can just calculate. But what’s the value of a mother seeing her child graduate? Of a man walking his daughter down the aisle after a cancer remission? The PBS doesn’t just price drugs - it tries to price dignity. And honestly? It’s doing better than most countries that call themselves 'free markets.'
Gregory Clayton
January 19, 2026 AT 18:05So Australia’s basically a socialist utopia now? Free medicine? No thanks. I’d rather pay $150 for a pill than live under a government that tells me what I’m allowed to buy. This is the beginning of the end. Next they’ll ban coffee because it’s 'too expensive for the poor.' 😤
Catherine Scutt
January 19, 2026 AT 18:52Who even is the PBAC? Some bureaucrats in a room deciding who lives and who doesn’t? Sounds like a dystopian novel. And don’t even get me started on the 14-month wait. That’s not policy - that’s cruelty dressed up as bureaucracy.
Darren McGuff
January 21, 2026 AT 17:28Interesting how the UK’s NICE has a harder cap than Australia’s PBAC. Makes you wonder - is flexibility a strength or a flaw? Australia’s system lets in more expensive drugs, sure, but at what cost? Longer waits, more pressure on the budget. The UK’s system is harsh, but it’s predictable. Ours feels like a lottery where the house always wins.
Johanna Baxter
January 22, 2026 AT 04:22My brother died waiting for a drug to be listed. 14 months. He was 32. The PBAC said it was 'not cost-effective.' So I guess his life wasn’t worth $150k. Good to know. 😔
Phil Kemling
January 23, 2026 AT 07:27If you think the PBS is about fairness, you’re ignoring the deeper question: Why do we let corporations own the patents on life-saving drugs in the first place? The system works because it’s a compromise - but the real problem is that medicine is treated like a product, not a right. The PBS patches the hole, but the dam is still cracked.
Diana Stoyanova
January 23, 2026 AT 23:58Okay real talk - I used to think PBS was just 'government help.' But after my mom got diagnosed with MS and we saw how the safety net kicked in after 8 months of spending? I got chills. That $7.70 co-pay? It’s not just money. It’s hope. It’s the difference between 'I can’t afford this' and 'I’ll be here to see my granddaughter’s wedding.' This isn’t policy. This is love made into law. And yeah, it’s messy. But it’s ours. Let’s fix it, not break it.
Elisha Muwanga
January 25, 2026 AT 18:24The PBS is a textbook example of government overreach. Subsidizing pharmaceuticals distorts market signals, encourages dependency, and creates perverse incentives for manufacturers to game the system. If Australians truly valued personal responsibility, they would pay full price and invest in private insurance - not rely on a bloated, inefficient state apparatus.