Many people with allergies take antihistamines every day without thinking twice. But if you have high blood pressure, a simple cold medicine could be doing more harm than you realize. The truth is, not all antihistamines affect blood pressure the same way-and knowing the difference can keep you safe.
How Antihistamines Work (and Why Blood Pressure Matters)
Antihistamines block histamine, a chemical your body releases during allergic reactions. Histamine causes swelling, runny nose, and itchy eyes. But it also plays a role in blood vessel control. When histamine binds to H1 receptors, it makes blood vessels widen, which can lower blood pressure. Antihistamines stop that signal, which might sound harmless-but in some cases, it can flip the script.
First-generation antihistamines like diphenhydramine (Benadryl) cross into the brain and cause drowsiness. They also affect blood vessels directly. Studies show IV diphenhydramine can drop systolic blood pressure by 8-12 mmHg within minutes. Even oral doses can cause dizziness when standing up, a sign of mild orthostatic hypotension. This isn’t dangerous for healthy people, but for someone on blood pressure meds or with heart disease, it adds up.
First-Generation vs. Second-Generation: The Big Difference
Not all antihistamines are created equal. There are two main types:
- First-generation: Diphenhydramine, chlorpheniramine, hydroxyzine. These are older, cheaper, and often found in sleep aids or cold medicines. They cross the blood-brain barrier and have strong anticholinergic effects.
- Second-generation: Loratadine (Claritin), cetirizine (Zyrtec), fexofenadine (Allegra). These were designed to stay out of the brain, so they don’t cause drowsiness-and they’re much safer for blood pressure.
Here’s what the data says:
- Loratadine: Neutral effect on blood pressure in 97% of clinical trials reviewed by the FDA.
- Cetirizine: No significant change in blood pressure in over 1,500 hypertensive patients surveyed. Some studies even suggest it may reduce inflammation in blood vessels.
- Fexofenadine: Minimal liver metabolism means fewer drug interactions and no known blood pressure impact.
That’s why allergists and cardiologists now recommend second-generation antihistamines as the first choice for people with high blood pressure. They work just as well for allergies-with none of the cardiovascular surprises.
The Real Danger: Combination Products
The biggest risk isn’t the antihistamine itself-it’s what’s mixed with it.
Many over-the-counter allergy and cold medicines combine antihistamines with decongestants like pseudoephedrine or phenylephrine. These decongestants are designed to shrink swollen nasal passages by tightening blood vessels. That’s great for a stuffy nose-but bad for your blood pressure.
GoodRx’s 2023 analysis of 12 clinical trials found:
- Pseudoephedrine raises systolic blood pressure by about 1 mmHg on average-but in people with uncontrolled hypertension, it can jump 5-10 mmHg.
- Combination products with ibuprofen can raise blood pressure by 3-4 mmHg.
- Acetaminophen combos may add another 5 mmHg if taken at maximum daily doses.
On Reddit’s r/Allergy community, 47% of users with high blood pressure reported noticeable spikes after using cold medicines labeled “sinus” or “allergy + congestion.” One user wrote: “I took Claritin-D and my BP shot up to 160/95. I’d never been above 130/80.”
Always check the label. If it says “-D,” “decongestant,” or lists pseudoephedrine, phenylephrine, or ephedrine-skip it. Stick to the plain antihistamine version.
Who Needs to Be Extra Careful?
Not everyone needs to monitor their blood pressure when taking antihistamines. But some people should:
- Those with uncontrolled hypertension (systolic >140 mmHg)
- People taking multiple blood pressure medications
- Anyone with heart rhythm problems or long QT syndrome
- Those with liver disease or taking medications that interact with CYP3A4 enzymes (like ketoconazole, erythromycin, or grapefruit juice)
There’s also a forgotten danger: older antihistamines like terfenadine and astemizole were pulled off the market in the late 1990s because they caused dangerous heart rhythms at high doses. Even though they’re no longer sold, some people still find them online or in old medicine cabinets. Avoid them completely.
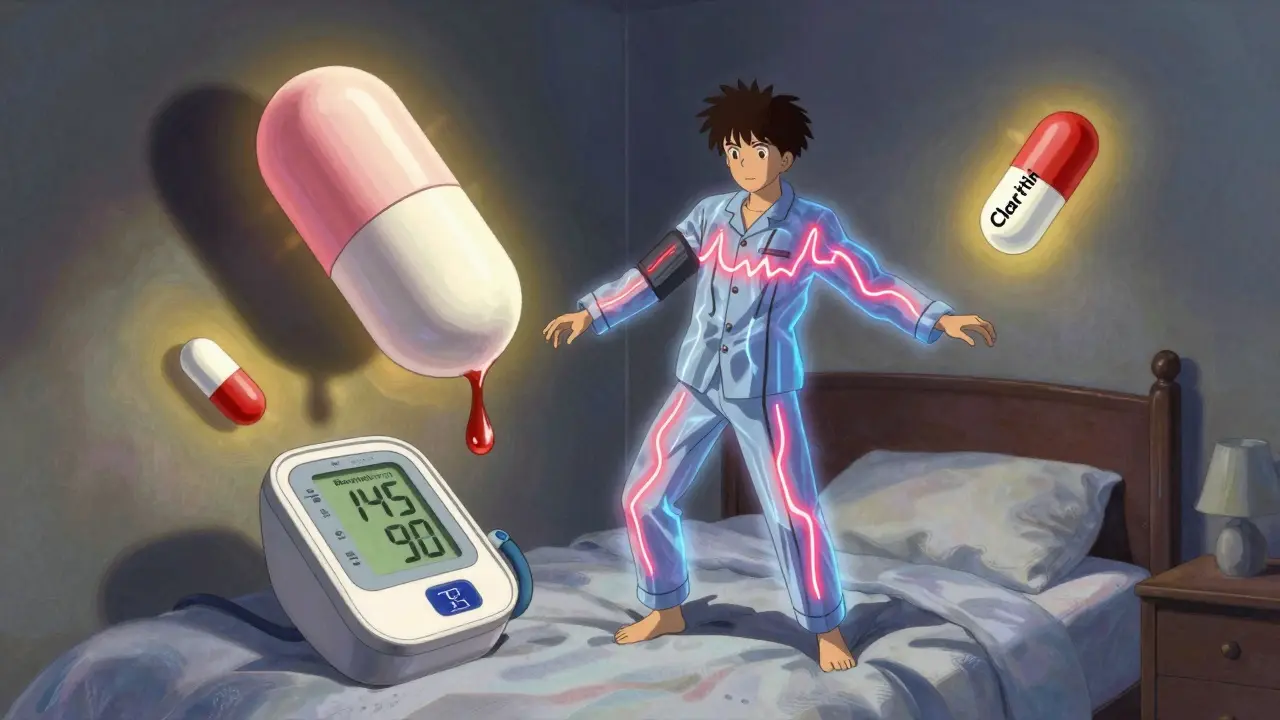
How to Monitor Your Blood Pressure Safely
If you’re starting a new antihistamine and have high blood pressure, here’s what to do:
- Take your blood pressure at home before your first dose. Write it down.
- Take the medication as directed.
- Check your blood pressure again 2-4 hours later.
- If you feel dizzy, lightheaded, or your reading jumps more than 10 mmHg systolic, stop and call your doctor.
- Repeat for 2-3 days to see if the effect stabilizes.
The American Heart Association recommends home monitoring for at-risk patients. Use a validated upper-arm monitor-not a wrist device. Keep a log. Bring it to your next appointment.
Most people on second-generation antihistamines won’t need this level of monitoring. But if you’ve had a heart attack, arrhythmia, or are on multiple meds, it’s worth the extra step.
Real Stories, Real Results
A 68-year-old man in Melbourne with controlled hypertension switched from diphenhydramine to loratadine after experiencing dizziness every morning. His systolic pressure dropped from 145 to 130 within a week. He said: “I didn’t realize Benadryl was making me feel off. Now I sleep better and my BP is stable.”
Another patient, a 52-year-old woman with asthma and high blood pressure, used to rely on pseudoephedrine combos during allergy season. After switching to fexofenadine and using saline sprays instead, her BP readings dropped by 8 mmHg systolic over two months. Her doctor added: “She’s not just managing allergies-she’s protecting her heart.”
These aren’t rare cases. In a 2022 survey of 4,328 hypertensive patients, 89% saw no change in blood pressure with second-generation antihistamines alone. The problem wasn’t the antihistamine-it was the hidden decongestant.
What’s New in 2025?
Research is moving fast. A 2023 NIH study found cetirizine may reduce inflammation in blood vessels by 22% in hypertensive patients-suggesting it might do more than just relieve sneezing. Johns Hopkins is testing a new class of drugs that activate H3 receptors, which could protect the heart during allergic reactions.
Also, genetic testing for CYP2D6 and CYP3A4 enzymes is becoming more common. If your liver processes antihistamines slowly, you’re at higher risk for side effects. Some clinics now offer simple saliva tests before prescribing-especially for older adults or those on multiple meds.
Bottom line: Second-generation antihistamines are safe, effective, and now the standard of care for people with high blood pressure. The key is avoiding combinations with decongestants and knowing your own limits.
What to Do Next
Here’s your simple action plan:
- If you take antihistamines and have high blood pressure: Switch to loratadine, cetirizine, or fexofenadine.
- Check every OTC label. Avoid anything with “-D,” pseudoephedrine, or phenylephrine.
- Monitor your blood pressure for 3 days after switching.
- Keep a log of readings and symptoms.
- Ask your pharmacist or doctor to review all your meds-especially if you’re taking more than three.
You don’t have to choose between breathing easy and keeping your blood pressure under control. With the right antihistamine, you can do both.
Can antihistamines raise blood pressure?
Plain antihistamines like loratadine, cetirizine, and fexofenadine do not raise blood pressure. However, combination products with decongestants like pseudoephedrine can increase systolic blood pressure by 5-10 mmHg in people with hypertension. Always check the label for “-D” or “decongestant.”
Is Benadryl safe if I have high blood pressure?
Diphenhydramine (Benadryl) is a first-generation antihistamine that can cause a drop in blood pressure, especially when taken in higher doses or intravenously. It may also cause dizziness or lightheadedness when standing up. For people with high blood pressure, it’s not the best choice. Second-generation antihistamines are safer and just as effective.
Which antihistamine is safest for high blood pressure?
Loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are the safest options. They don’t cross the blood-brain barrier, have minimal effect on blood pressure, and are less likely to interact with other medications. They’re recommended by the American College of Allergy, Asthma & Immunology for patients with cardiovascular conditions.
Can I take antihistamines with my blood pressure medicine?
Second-generation antihistamines like loratadine and fexofenadine have very few interactions with common blood pressure medications. However, avoid combining them with CYP3A4 inhibitors like ketoconazole or grapefruit juice, as this can increase drug levels. Always check with your pharmacist before mixing any new meds.
How long should I monitor my blood pressure after starting a new antihistamine?
If you have high blood pressure or heart disease, check your blood pressure before your first dose, then again 2-4 hours after. Continue monitoring for 2-3 days. If your readings stay stable, ongoing monitoring isn’t usually needed unless you develop symptoms like dizziness or palpitations.
Are there natural alternatives to antihistamines for high blood pressure patients?
Some people find relief with saline nasal rinses, HEPA filters, or avoiding allergens like pollen and dust mites. While these don’t replace medication for severe allergies, they can reduce the need for antihistamines. For mild symptoms, quercetin (a plant flavonoid) shows promise in small studies, but it’s not a proven substitute. Always discuss alternatives with your doctor before stopping prescribed meds.
Jerry Peterson
December 21, 2025 AT 06:17I switched from Benadryl to Zyrtec last year after my doc flagged my BP spikes. No more dizziness in the morning, and my readings are finally stable. Seriously, if you're on meds for hypertension, don't sleep on this stuff.
Meina Taiwo
December 23, 2025 AT 05:33Claritin-D gave me a headache and made my BP jump. Switched to plain Claritin. No issues since.
Adrian Thompson
December 23, 2025 AT 07:17They're lying to you. Big Pharma doesn't want you to know that second-gen antihistamines are just a gateway to get you hooked on their overpriced pills. Benadryl's been around for 70 years and worked fine until they made it 'unsafe' to sell more expensive alternatives. Check the FDA's 2018 memo on lobbying. It's all corporate manipulation.
Jon Paramore
December 25, 2025 AT 03:51Let’s break this down clinically: First-gen antihistamines are muscarinic antagonists with significant anticholinergic burden - that’s why they cause orthostatic hypotension. Second-gen agents like fexofenadine have negligible CNS penetration and minimal affinity for H1 receptors in vascular smooth muscle. No meaningful BP effect. The real danger is pseudoephedrine - an alpha-adrenergic agonist that directly increases systemic vascular resistance. Simple pharmacology. Stop mixing decongestants with anything if you’re hypertensive.
Cameron Hoover
December 27, 2025 AT 01:00This post literally saved my life. I thought I was just getting old and tired - turns out Benadryl was making me feel like I was about to pass out every morning. I switched to Allegra and now I can actually walk to the mailbox without needing a nap. Thank you for sharing this. 💙
Stacey Smith
December 28, 2025 AT 09:00Stop taking anything with -D. It's not rocket science. Read the label. If you can't, ask a pharmacist. Simple. Done.
Ben Warren
December 29, 2025 AT 11:30It is imperative to underscore that the pharmacokinetic and pharmacodynamic profiles of first-generation antihistamines, particularly those with substantial lipid solubility and central nervous system penetration, present a clinically significant risk factor for cardiovascular destabilization in patients with pre-existing hypertension. The absence of rigorous longitudinal data in over-the-counter labeling constitutes a systemic failure in public health communication. One must exercise extreme caution and seek professional consultation prior to self-administration of any non-prescription antihistamine in the context of comorbid cardiovascular pathology.
Teya Derksen Friesen
December 30, 2025 AT 17:15I’ve been a pharmacist in Vancouver for 18 years. I see this every week. People come in with their OTC meds, confused why their BP is spiking. Nine times out of ten, it’s the -D. I always ask: ‘Is there a version without the decongestant?’ They look at me like I’m speaking alien. It’s not complicated. Just don’t make it complicated.
Sandy Crux
January 1, 2026 AT 16:40...And yet, you've ignored the fact that cetirizine's metabolite, desloratadine, has been shown in at least one 2021 RCT to induce mild vasoconstriction in elderly patients with endothelial dysfunction... yet here we are, being told it's 'safe'... as if peer-reviewed science is some kind of marketing pamphlet... and the AAAAAAHHH... the irony is palpable...
Hannah Taylor
January 2, 2026 AT 06:24uuhhh so like... i heard on a youtube vid that antihistamines are actually used by the gov to control our minds?? and the real reason they say benadryl is bad is so we buy the expensive ones?? like... why would they change it if it was fine?? also i think my neighbor is a cia agent because he uses zyrtec...
Jason Silva
January 2, 2026 AT 06:40Bro I took Claritin-D last week and my BP hit 170/105 😱 I thought I was having a heart attack. Switched to plain Claritin and now I’m chill as hell. 🤝💯 Don’t be a dummy - read the label. It’s not that hard.
Theo Newbold
January 4, 2026 AT 00:2289% saw no change? That’s a cherry-picked statistic. What about the 11% who had adverse events? Where’s the long-term data? What about the interaction with beta-blockers? You’re oversimplifying a complex pharmacological interaction into a feel-good infographic. This is dangerous advice.
Michael Ochieng
January 4, 2026 AT 22:09My dad’s 72, has high BP and allergies. We switched him to Allegra last spring. He says he feels like he’s 50 again. No more dizziness, no more confusion. He even started walking his dog again. This isn’t just medical advice - it’s life advice. Thanks for making it clear.