Anticoagulant Bleeding Risk Calculator
This calculator helps you understand your bleeding risk when taking anticoagulants. Based on data from clinical studies, it provides an estimate of your relative bleeding risk compared to the average patient.
Your Bleeding Risk Assessment
Personalized Recommendations
Why Anticoagulants Can Be Dangerous - And How to Stay Safe
Anticoagulants save lives. They prevent strokes in people with atrial fibrillation, stop deadly clots in the legs and lungs, and protect those with mechanical heart valves. But for every life they save, they carry a real risk: uncontrolled bleeding. About 1 to 3% of people on these drugs each year will have a major bleed - some fatal. The goal isn’t to avoid anticoagulants. It’s to use them wisely so the benefits far outweigh the dangers.
What Anticoagulants You’re Likely Taking - And How They Differ
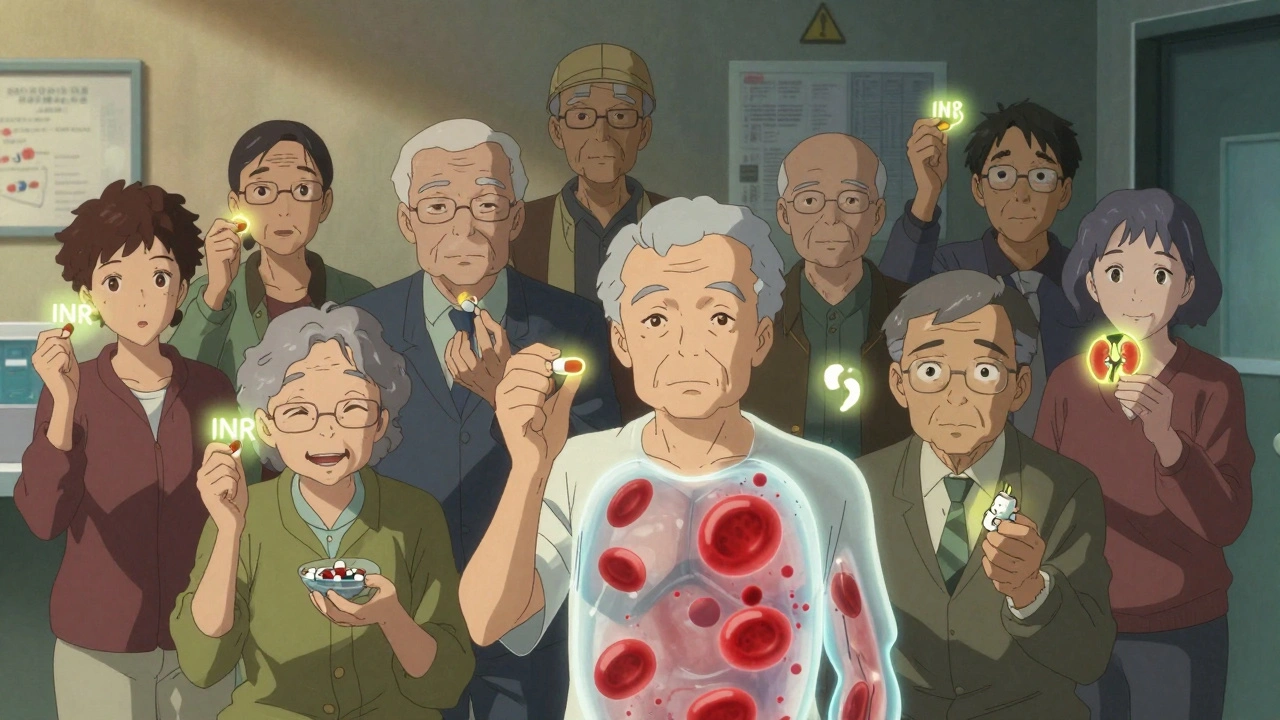
There are three main types of blood thinners used today. Warfarin has been around since the 1950s. It works by blocking vitamin K, which your body needs to make clotting factors. But it’s finicky. You need regular blood tests (INR) to make sure your dose is right. If your INR is too high, you bleed. Too low, and you’re at risk for a clot. Keeping your INR between 2.0 and 3.0 is critical - and even then, each 10% drop in the time you spend in that range increases your bleeding risk by 15%.
Most people now take DOACs - direct oral anticoagulants. These include apixaban, rivaroxaban, dabigatran, and edoxaban. They don’t need regular blood tests. Dosing is fixed. But they’re not perfect. They rely on your kidneys to clear them from your body. If your kidney function drops - which happens naturally with age - drug levels can build up, raising bleeding risk. Apixaban is the safest in this group, with a 31% lower risk of major bleeding than warfarin in clinical trials. Rivaroxaban and edoxaban require dose adjustments if your creatinine clearance falls below 50 mL/min. Dabigatran needs a lower dose if your kidney function is below 30 mL/min.
Heparin and its cousins (like enoxaparin) are used mostly in hospitals or right after surgery. They work fast but need injections and monitoring. They can also cause a rare but serious side effect called heparin-induced thrombocytopenia, where your body forms clots instead of preventing them.
Who’s at Highest Risk for Bleeding?
Not everyone on anticoagulants has the same risk. Age is the biggest factor. People over 75 bleed two to three times more often than younger adults. Kidney problems double the risk. Liver disease, uncontrolled high blood pressure, and a history of prior bleeding all raise the odds. And if you’re taking aspirin, clopidogrel, or other antiplatelet drugs along with your anticoagulant? Your bleeding risk jumps by 50 to 70%.
Women on anticoagulants who undergo procedures like first-trimester abortions may experience heavier bleeding than expected. Studies show some see hemoglobin drops below 7 g/dL - enough to need a transfusion. That’s why doctors now screen for anticoagulant use before any procedure, even minor ones.

How to Prevent Bleeding - Practical Steps
- Know your kidney function. Get your creatinine clearance checked when you start the drug, then every 3 to 6 months. If it drops, your dose may need adjusting - especially for DOACs.
- Avoid dual therapy. Don’t take aspirin or NSAIDs like ibuprofen unless your doctor specifically says so. Even low-dose aspirin increases bleeding risk significantly.
- Don’t skip doses or stop early. Stopping anticoagulants suddenly can cause clots. If you miss a dose, check your drug’s guidelines. DOACs are forgiving - if you miss one, take it within 6 to 12 hours. Warfarin? Don’t double up. Call your doctor.
- Watch for signs of bleeding. Unexplained bruising, pink or red urine, black or tarry stools, vomiting blood, severe headaches, or sudden weakness could mean internal bleeding. Don’t wait. Go to the ER.
- Use a medication reminder. Elderly patients are more likely to make dosing errors. A pill organizer or phone alert can prevent accidental overdoses.
What Happens If You Bleed - And How Doctors Reverse It
Emergency reversal depends on what drug you’re taking. For warfarin, the fastest fix is a four-factor prothrombin complex concentrate (4f-PCC). It works in 15 minutes. Fresh frozen plasma takes hours and requires thawing - not ideal in a crisis. Vitamin K helps too, but it takes 8 to 24 hours to kick in.
For dabigatran, there’s a specific antidote: idarucizumab. Given as two vials IV, it reverses the drug in minutes. For apixaban, rivaroxaban, and edoxaban, andexanet alfa is the reversal agent. It’s expensive - about $13,000 per dose - and not always available. But when you’re bleeding out, cost doesn’t matter. Time does.
For heparin, protamine sulfate is the antidote. It neutralizes most of the drug, but it doesn’t work well for low-molecular-weight heparins like enoxaparin. In those cases, doctors may wait for the drug to clear naturally - which takes 12 to 24 hours.
When to Restart Anticoagulation After a Bleed
This is one of the hardest decisions doctors face. Stop too soon, and you risk a stroke or pulmonary embolism. Restart too fast, and you bleed again.
Guidelines say: if your risk of clotting is low - like someone with a provoked blood clot that happened months ago and a CHA₂DS₂-VASc score under 3 - you might not need to restart. But if you have atrial fibrillation, a mechanical valve, or a history of unprovoked clots, restarting is usually the right move. Most patients can restart within 1 to 2 weeks after a minor bleed. For major bleeds, like brain or gastrointestinal bleeding, doctors wait 4 to 8 weeks - but not longer than that. The longer you wait, the higher your risk of a clot.
The Future: Better Tools, Fewer Bleeds
Scientists are working on universal reversal agents. One called ciraparantag is in trials and could neutralize all major anticoagulants with a single shot. If it works, it could cut emergency deaths from bleeding by 20% or more.
Point-of-care tests for DOACs are also coming. Right now, there’s no quick way to measure if apixaban or rivaroxaban levels are too high. New devices may soon give results in minutes - like an INR test for warfarin. That could prevent many overdoses before they happen.
And then there’s personalized dosing. Genetic testing can now predict how someone will respond to warfarin. Some people need half the dose because of how their liver processes it. That’s not routine yet - but it’s coming.
Bottom Line: Anticoagulants Are Powerful - But Not Dangerous If You’re Informed
You don’t need to fear anticoagulants. You need to respect them. They’re not one-size-fits-all. Your age, kidney function, other medications, and medical history all matter. Work with your doctor to pick the right one. Get regular check-ups. Know the signs of bleeding. And never stop taking them without talking to your provider.
The goal isn’t to avoid bleeding entirely. It’s to live safely with your condition - whether it’s atrial fibrillation, a history of clots, or a mechanical valve - without letting fear stop you from living well.
Can I take ibuprofen or aspirin while on anticoagulants?
Generally, no. Combining NSAIDs like ibuprofen or naproxen with anticoagulants increases your risk of stomach bleeding by up to 70%. Aspirin, even low-dose, does the same. If you need pain relief, acetaminophen (paracetamol) is usually safer. Always check with your doctor before taking any new medication.
Do DOACs require blood tests like warfarin?
No, DOACs don’t need routine INR testing. That’s one reason they’re preferred for most patients. But your kidney function still needs monitoring - typically every 3 to 6 months. If you have kidney disease, your doctor may check more often. Some hospitals now offer special tests to measure DOAC levels in emergencies, but these aren’t used for routine care.
What if I need surgery or a dental procedure?
Never stop your anticoagulant without talking to your doctor. For minor procedures like tooth extractions, you usually don’t need to stop. For major surgery, your doctor may pause it for a day or two, depending on the drug and your clotting risk. DOACs are often stopped 24 to 48 hours before surgery. Warfarin may need to be stopped 5 days prior, with bridging heparin used in high-risk cases. Always coordinate between your surgeon and prescribing doctor.
Is one anticoagulant safer than the others?
Apixaban has the lowest bleeding risk among DOACs, based on large clinical trials. It’s also less affected by kidney problems than rivaroxaban or edoxaban. But safety depends on your individual situation. For mechanical heart valves or antiphospholipid syndrome, warfarin is still the only proven option. Your doctor will pick the best fit for your health profile, not just the safest on paper.
Can I drink alcohol while on anticoagulants?
Moderate alcohol is usually okay - one drink per day for women, two for men. But heavy drinking can interfere with how your liver processes warfarin, making your INR unstable. It can also irritate your stomach lining, increasing bleeding risk. If you drink regularly, tell your doctor. They may need to monitor you more closely.
What should I do if I fall and hit my head?
Even if you feel fine, go to the ER. Anticoagulants increase the risk of bleeding inside the skull, which can be silent at first. A headache, dizziness, confusion, or vomiting after a head injury could mean internal bleeding. Don’t wait. Get a CT scan. It’s better to be safe than sorry.
john damon
December 10, 2025 AT 14:31matthew dendle
December 10, 2025 AT 18:59Michelle Edwards
December 11, 2025 AT 14:07Taylor Dressler
December 13, 2025 AT 11:50Aidan Stacey
December 13, 2025 AT 17:15Rebecca Dong
December 14, 2025 AT 01:14Sarah Clifford
December 14, 2025 AT 12:35Regan Mears
December 16, 2025 AT 03:55Ben Greening
December 16, 2025 AT 17:48Nikki Smellie
December 17, 2025 AT 06:02