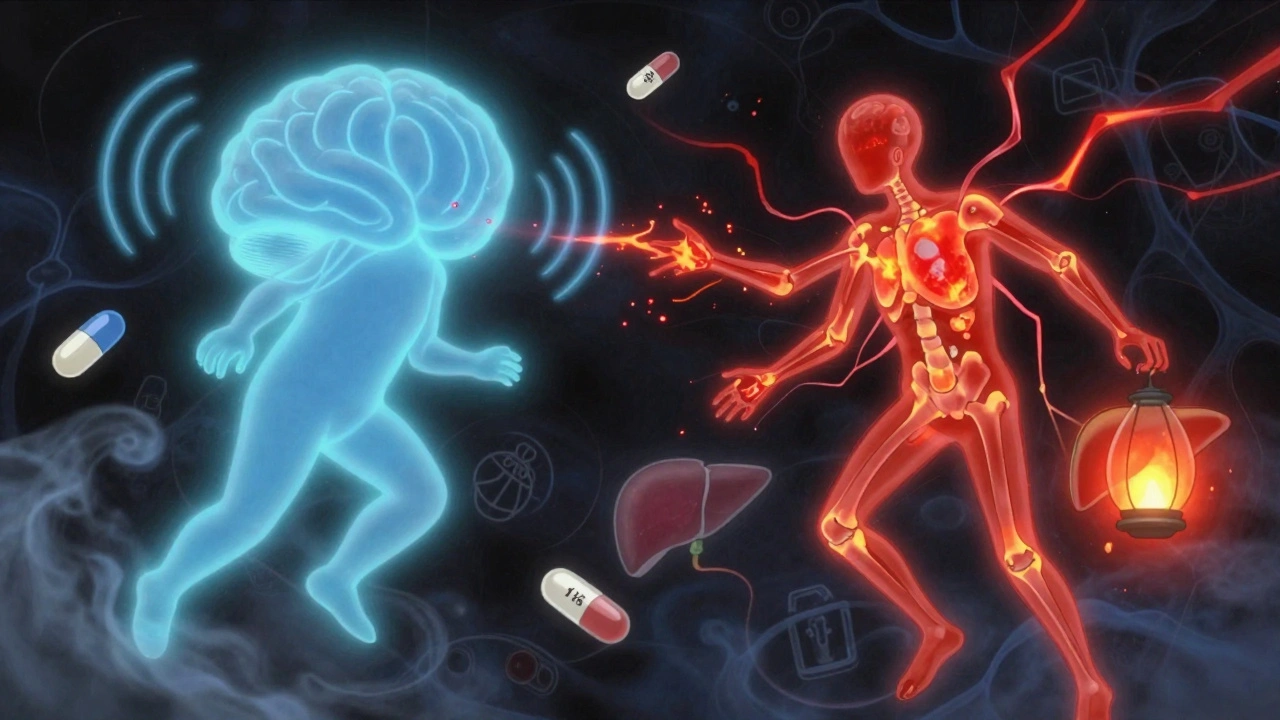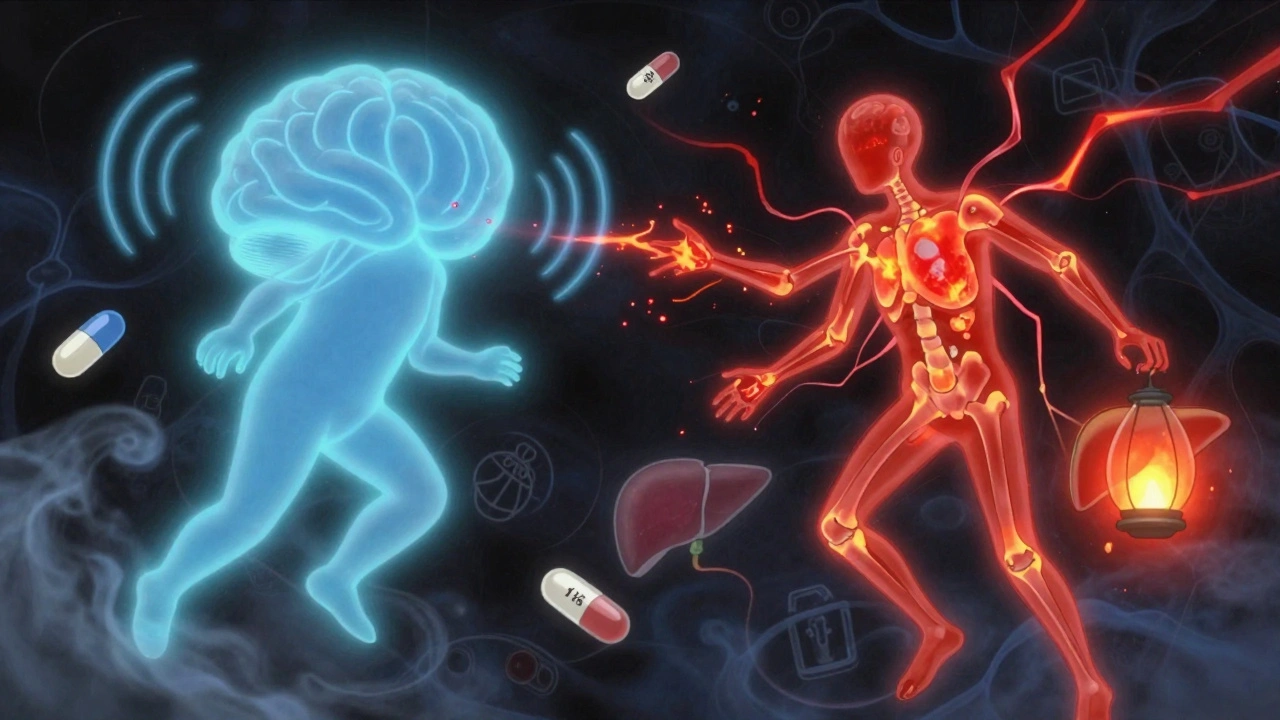
Pain Medication Comparison: What Works, What Risks, and What to Avoid
When you reach for a pain reliever, you’re not just picking a pill—you’re choosing a pain medication, a drug designed to reduce or block pain signals in the body. Also known as analgesics, these medications range from over-the-counter staples like ibuprofen to powerful prescriptions like oxycodone, and each carries its own set of trade-offs. The right one for you depends on the type of pain, how long you’ve had it, your medical history, and even what other drugs you’re taking.
Take NSAIDs, a class of drugs that reduce inflammation and pain by blocking enzymes linked to swelling. Also known as nonsteroidal anti-inflammatory drugs, they include common names like ibuprofen and naproxen. They work great for muscle aches, arthritis, or menstrual cramps—but they can wreck your stomach lining or raise your blood pressure if used too long. Then there’s acetaminophen, a painkiller that doesn’t reduce inflammation but is gentler on the stomach. Also known as paracetamol, it’s safer for daily use—but overdose it, even by a little, and you risk liver failure. And then there are opioids, strong drugs that bind to brain receptors to shut down pain signals. Also known as narcotics, they’re powerful for severe pain after surgery or cancer—but they’re also addictive, and misuse can lead to overdose. You don’t need to take opioids for a headache. But if you have chronic back pain or nerve pain, they might be part of a plan—only if other options fail.
Some pain meds are designed for specific conditions. For example, triptans, a type of migraine-specific drug that narrows blood vessels in the brain. Also known as migraine abortives, they stop a headache in its tracks—but they’re useless for a toothache or sprained ankle. And while some people turn to steroids for joint pain, those aren’t pain meds in the traditional sense—they’re anti-inflammatories with long-term side effects. Even herbal options like turmeric or capsaicin cream have real data behind them, but they don’t work like a pill. They work slowly, and only for some people.
What you won’t find in this collection is a one-size-fits-all answer. That’s because pain isn’t one thing. It’s sharp or dull, sudden or lasting, caused by injury, inflammation, or nerve damage. The same drug that helps your back pain might do nothing for your migraine—or make it worse. You’ll find real comparisons here: how ibuprofen stacks up against naproxen, why some people can’t take NSAIDs at all, how acetaminophen is safer for the stomach but riskier for the liver, and when opioids are truly necessary versus when they’re overprescribed.
Some of these posts dig into the hidden dangers: how mixing alcohol with pain meds can slow your breathing to a stop, why switching generic versions of certain drugs like phenytoin can trigger seizures, and how long-term use of painkillers can damage your kidneys or lead to rebound headaches. Others show you alternatives: what works for nerve pain when opioids fail, how topical creams can replace pills for joint pain, and why some people find relief with non-drug methods like physical therapy or nerve blocks.
There’s no magic bullet. But there is a smarter way to choose. You don’t have to guess. You don’t have to rely on what your friend swears by. You can see the facts—side effects, effectiveness rates, drug interactions, and real-world risks—side by side. What you’re about to read isn’t just a list of pills. It’s a map to help you avoid the traps, pick the right tool, and stay safe while you manage your pain.