OTC Pain Relievers: What Works, What to Avoid, and How to Use Them Safely
When you have a headache, sore muscles, or a fever, OTC pain relievers, over-the-counter medications used to reduce pain and fever without a prescription. Also known as non-prescription analgesics, they’re the first line of defense for millions of people every day. But just because you can buy them off the shelf doesn’t mean they’re harmless. Every year, thousands end up in the ER because they took too much, mixed them with other drugs, or didn’t realize they had an underlying condition that made these meds dangerous.
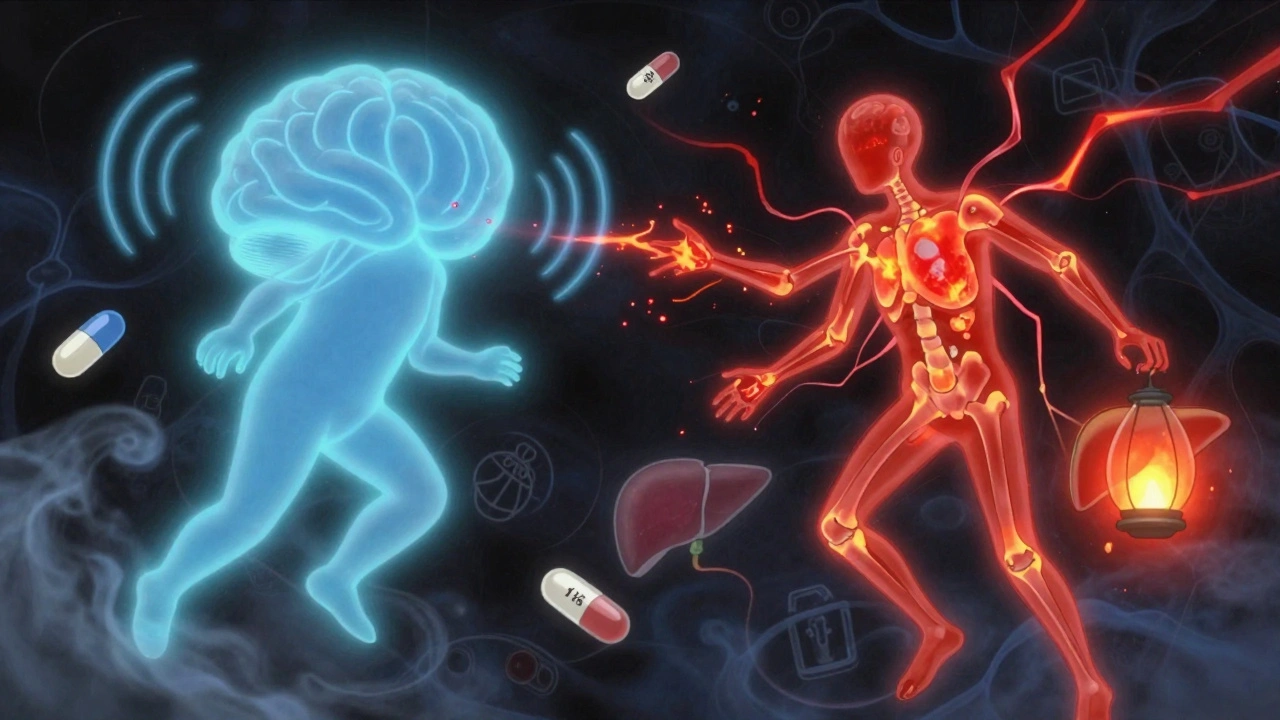
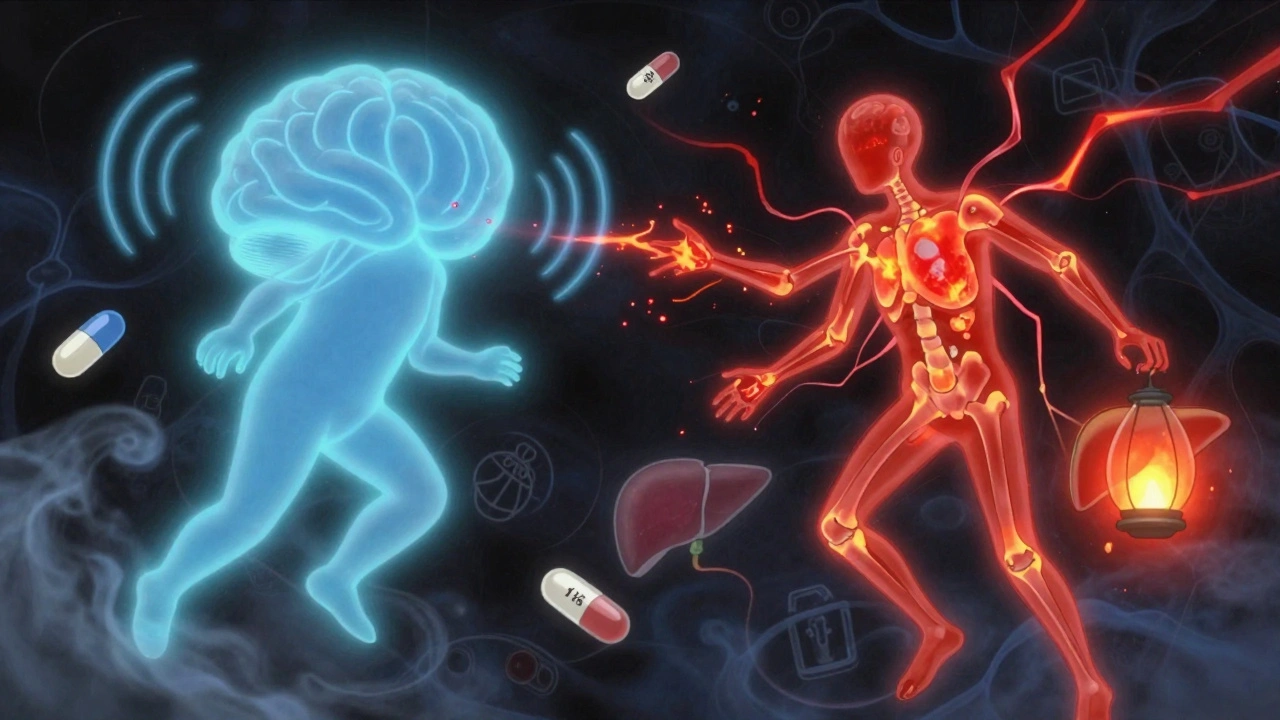
Two main types dominate the market: NSAIDs, nonsteroidal anti-inflammatory drugs that reduce inflammation, pain, and fever like ibuprofen and naproxen, and acetaminophen, a pain reliever and fever reducer that doesn’t fight inflammation. NSAIDs work by blocking enzymes that cause swelling and pain, but they also weaken the stomach’s protective lining—this is why they’re linked to gastrointestinal bleeding, especially in older adults or people with ulcers. Acetaminophen doesn’t hurt your stomach, but it’s hard on your liver. Take more than directed, or mix it with alcohol, and you risk serious, sometimes fatal, liver damage.
Many people think they can safely take these meds every day if they feel okay. But long-term use of OTC pain relievers—even at normal doses—can quietly damage your kidneys, raise your blood pressure, or mask symptoms of something more serious like an infection or early arthritis. If you’re using them more than a few days a week, it’s not just a habit—it’s a signal. Something in your body needs attention, not just masking.
And it’s not just about dosage. Timing matters. Taking NSAIDs on an empty stomach? That’s asking for trouble. Mixing them with blood thinners or antidepressants? That’s a recipe for complications. Even your coffee can interfere—some studies show caffeine can make pain relievers work faster, but it can also increase the risk of stomach irritation when combined with NSAIDs.
What you’ll find in the posts below isn’t just a list of brands or dosages. It’s real-world insight into how these drugs behave in your body, who’s most at risk, and what alternatives actually work. You’ll see how NSAIDs connect to ulcers, why acetaminophen is safer for some but deadly for others, and how to spot early signs of damage before it’s too late. There’s also advice on when to skip OTC meds entirely and how to talk to your pharmacist about safer options.
This isn’t about scaring you off pain relief. It’s about giving you the facts so you can use these common drugs without becoming a statistic. Whether you’re managing daily aches, recovering from an injury, or just trying to get through the day, knowing how these pills work—and when they don’t—is the difference between feeling better and getting worse.