When you see an FDA safety alert about a medication you’re taking, it’s natural to panic. Maybe your doctor just prescribed it. Maybe you’ve been on it for years. Now you’re reading words like "potential signal," "serious risk," or "new safety information." What does that actually mean? Should you stop taking it? Is this a real danger or just noise? The truth is, most people - even some doctors - misinterpret these announcements. And that’s not because they’re not smart. It’s because the FDA doesn’t always explain things clearly.
What the FDA Actually Means by "Potential Signal"
The FDA doesn’t issue safety alerts because they’ve proven a drug is dangerous. They issue them because they’ve seen something unusual in the data - a pattern that needs more investigation. The term "potential signal" is the key. It means: "We noticed something odd. We’re not sure yet if it’s real. But we’re watching." For example, in Q3 2023, the FDA reported a potential signal linking a common diabetes drug to a rare skin infection called Fournier’s gangrene. That sounds terrifying. But here’s the real context: out of every 1,000 people taking the drug for a year, about 0.2 cases occurred. Compare that to the 0.06 cases per 1,000 people not taking it. The risk went up - but it was still extremely rare. The FDA didn’t say "don’t take this drug." They said: "We’re looking into this. If you have diabetes and are on this drug, watch for sudden pain or swelling in the genital area. If it happens, get help right away." This is the difference between a signal and a confirmed risk. A signal is a red flag on a radar screen. A confirmed risk is the enemy plane on the radar. Most FDA alerts are just the first flicker.Why Your Doctor Might Be Confused Too
A 2022 survey of 1,200 doctors found that 68% felt FDA safety communications "lack sufficient context about the magnitude of risk." That’s not a small number. It means nearly seven out of ten clinicians don’t feel equipped to explain these alerts to patients. Take the 2023 alert about SSRIs and pregnancy. The FDA said there was a "potential signal" of increased risk for certain birth defects. But they didn’t say by how much. So doctors got flooded with anxious patients. One doctor on Reddit said 12 of her patients called in a panic - all because the alert didn’t mention that the absolute risk increase was less than 1%. Meanwhile, untreated depression during pregnancy carries risks to both mother and baby that are far more common and serious. The FDA’s job is to catch rare, serious problems. But they don’t always explain how rare. That’s where the confusion comes in. You can’t compare a 0.02% risk to a 20% risk without numbers. And too often, those numbers are missing.How to Read an FDA Alert Like a Pro
You don’t need to be a scientist to understand these alerts. You just need to ask three questions:- Is this a "potential signal" or a "confirmed risk"? Look for those exact phrases. If it says "potential signal," the FDA hasn’t proven causation. If it says "confirmed risk," they have strong evidence. Only about 40% of alerts are confirmed risks.
- How serious is the risk? The FDA defines "serious" as something that’s fatal, life-threatening, requires hospitalization, or causes permanent disability. If the risk is a headache or mild nausea, it’s not a reason to stop the drug.
- What’s the benefit? Are you taking this drug for high blood pressure, or for a life-threatening cancer? The risk-benefit balance changes completely. A drug with a 1% risk of liver damage might be perfectly reasonable for someone with terminal cancer - but not for someone with mild anxiety.
One of the best examples of clear communication came in August 2022, when the FDA issued an alert about SGLT2 inhibitors and Fournier’s gangrene. They didn’t just say "possible risk." They said: "Estimated incidence: 0.2 cases per 1,000 patient-years. Baseline risk in non-users: 0.06." That’s transparency. That’s useful.

Don’t Stop Your Medication Without Talking to Your Doctor
This is the most important thing: the FDA almost never tells you to stop taking a drug. Their standard language is: "Do not change your treatment without talking to your healthcare provider." Why? Because stopping a medication can be more dangerous than the risk itself. If you stop your blood pressure medicine because of a vague safety alert, you could have a stroke. If you stop your insulin because of a rare side effect, you could go into diabetic ketoacidosis. The risk of stopping often outweighs the risk of continuing. In 2021, the FDA issued an alert about menstrual changes after the COVID-19 vaccine. It caused widespread panic. Women stopped getting vaccinated. Later, the FDA clarified: the changes were temporary, common, and not linked to long-term fertility issues. The alert had been misinterpreted. The lesson? Don’t act on fear. Act on facts - and talk to your provider.What the FDA Isn’t Telling You (But You Need to Know)
There are three hidden truths about FDA safety alerts:- Most reports are incomplete. The FDA gets over 1.2 million adverse event reports a year. Many are from patients who don’t know if the drug caused the issue. Others are from people who took multiple drugs. The system is designed to catch signals - not prove causes.
- Benefit-risk changes over time. A drug that was safe for 10,000 people in a trial might show a new risk when used by 2 million people over 10 years. That’s why post-market surveillance matters. It’s not a failure - it’s the system working.
- Your doctor’s judgment matters more than the alert. The FDA gives you data. Your doctor gives you context. They know your health history, your other medications, your goals. That’s why they’re paid the big bucks.
Dr. Robert Temple, former FDA deputy director, put it simply: "The absence of evidence is not evidence of absence." But the reverse is also true: "The presence of a signal is not evidence of harm."
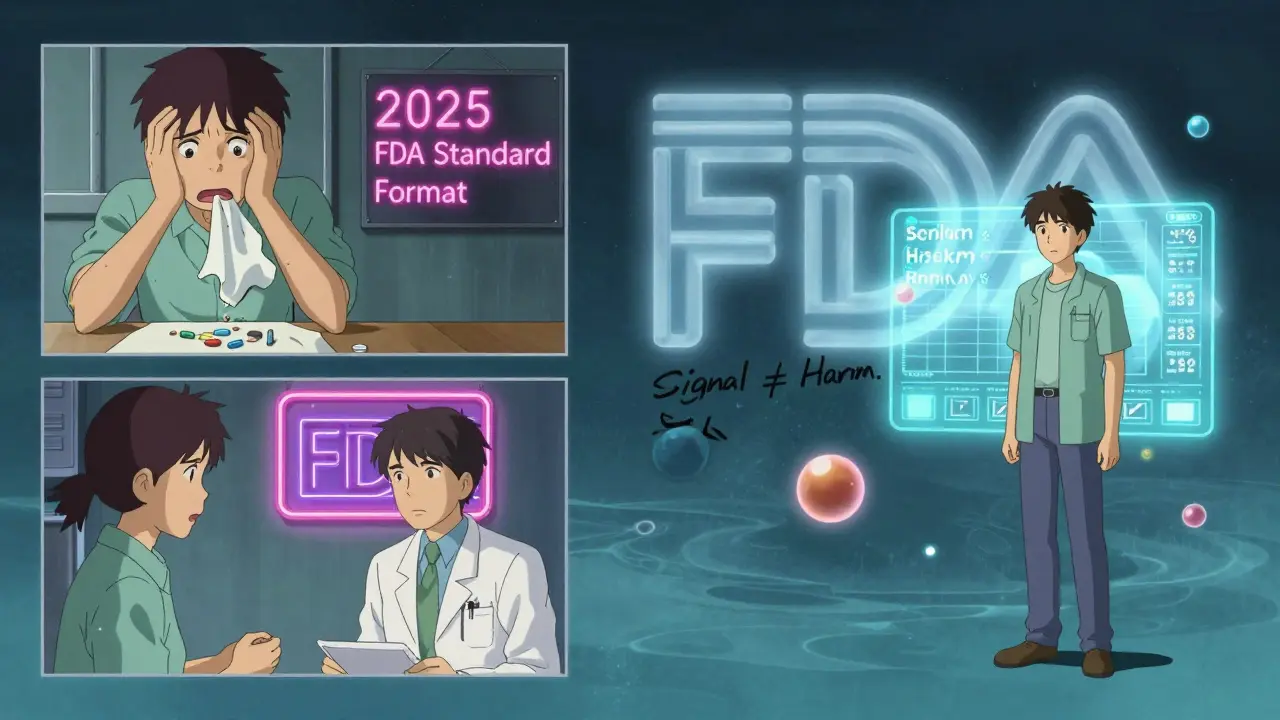
What’s Changing in 2025 and Beyond
The FDA knows its alerts are confusing. That’s why they’re changing. By Q3 2025, they’ll start using standardized formats that include:- Quantitative risk estimates (e.g., "1 in 5,000")
- Comparison to baseline risk (e.g., "This is 3x higher than the general population")
- Clear action steps: "Continue as is," "Monitor for X," or "Consider alternatives."
They’re also building a patient-facing tool that will let you plug in your condition and medication to see a visual risk-benefit chart. This is huge. It means you won’t have to guess anymore.
For now, the best advice is simple: read the alert. Understand the difference between signal and confirmed risk. Ask your doctor: "What’s the actual risk? How does it compare to the benefit? Should I change anything?" And don’t stop your meds just because of a headline.
Does the FDA issue safety alerts for every side effect?
No. The FDA only issues alerts for serious, unexpected, or newly discovered risks that could outweigh the drug’s benefit. Minor side effects like headaches, nausea, or dizziness are not reported unless they’re unusually common or linked to a serious outcome. The system is designed to catch life-threatening or disabling risks - not everyday discomforts.
Why do some drugs get alerts while others don’t, even if they have similar side effects?
It’s not just about the side effect - it’s about the context. A drug for a life-threatening illness like cancer might be allowed to have a higher risk profile than one for mild acne. Also, if a side effect was already known and listed in the label, the FDA won’t issue a new alert. Alerts are for new or unexpected risks. Two drugs may have the same side effect, but if one was approved 20 years ago and the other just last year, the newer one is more likely to trigger an alert because it’s still being monitored closely.
Can I trust the FDA’s safety alerts if they sometimes cause panic?
Yes - but you need to read them carefully. The FDA’s goal is to protect public health by catching rare dangers early. The panic comes from how the media or patients interpret the alerts, not from the FDA’s intent. The agency has improved its language significantly since 2020. Many alerts now include clear phrases like "this does not mean the drug causes this risk" and "do not stop taking your medication." The system isn’t perfect, but it’s the most rigorous in the world.
How long does it take for the FDA to confirm a risk after a signal?
It can take 6 to 18 months. Detecting a signal is fast - sometimes within weeks. But proving causation takes time. The FDA needs to rule out other causes, gather more data from real-world use, and often wait for peer-reviewed studies. This delay is intentional. It prevents overreaction. If the FDA acted on every signal immediately, we’d see drugs pulled from the market based on incomplete data - which has happened before and caused real harm.
What should I do if I experience a side effect mentioned in an FDA alert?
First, don’t panic. Second, don’t stop the medication on your own. Third, contact your doctor. Tell them exactly what you’re experiencing, when it started, and that you saw the FDA alert. Your doctor can assess whether it’s related to the drug, how serious it is, and whether any action is needed. In most cases, it’s not. But if it is, your doctor can help you switch safely.
Final Takeaway: It’s About Context, Not Fear
FDA safety alerts aren’t warnings to run away. They’re notifications to pay attention. They’re part of a system designed to catch rare dangers before they become widespread tragedies. But they’re not designed to scare you. They’re designed to inform - if you know how to read them.Every drug has risks. Every drug has benefits. The goal isn’t to find a drug with zero risk - that doesn’t exist. The goal is to find the right balance for you. And that’s not something you can figure out from a headline. It’s something you figure out with your doctor, your health history, and a little bit of clear thinking.

Brandon Osborne
February 10, 2026 AT 01:07Let me tell you something - this whole FDA thing is a circus. You think they’re trying to help? Nah. They’re covering their asses while you’re out here scared to take your blood pressure meds because some dude in a lab saw two people get a rash. I’ve been on metformin for 12 years. My A1C’s perfect. Now I’m supposed to panic because some ‘potential signal’? Bullshit. They don’t even say how rare. They just drop the bomb and vanish. Then the media turns it into a horror movie. And you? You’re left wondering if your insulin is gonna turn you into a vampire.
Lyle Whyatt
February 10, 2026 AT 11:05Man, I’ve been reading these FDA alerts for years now - and honestly, the system’s way more nuanced than most people realize. The key is understanding that ‘potential signal’ doesn’t mean ‘dangerous’ - it means ‘we saw something odd enough to flag.’ Like, if you’re driving and your car’s check engine light flickers? You don’t immediately sell the car. You check the code. The FDA’s doing the same thing. They’re not saying ‘stop the drug.’ They’re saying ‘we’re watching this closely.’ And yeah, they suck at communicating it. The 0.2 per 1,000 example? That’s gold. Most people don’t realize that’s less likely than being struck by lightning twice in your life. Context is everything. Without it, you’re just reacting to fear. With it? You’re making informed choices.
Tatiana Barbosa
February 10, 2026 AT 16:36As someone who’s been in the med space for over a decade, I can tell you - the FDA’s not the enemy. The real problem? The lack of quantified risk. They say ‘potential signal’ and assume we all know what that means. We don’t. I’ve had patients cry because they read ‘birth defect risk’ and didn’t know the absolute increase was 0.8%. That’s not panic - that’s a communication failure. We need plain language. We need numbers. We need ‘this is 3x higher than baseline’ not ‘we’re investigating.’ And yeah, doctors are clueless too - we’re all just trying to translate jargon into human. The fact that they’re rolling out visual risk-benefit charts in 2025? That’s the future. Finally.
Susan Kwan
February 11, 2026 AT 18:42Wow. This post is basically a PSA for people who think ‘FDA alert’ means ‘your life is over.’ Let me guess - you also think ‘potential signal’ is code for ‘the government is poisoning us.’ Newsflash: if the FDA wanted to kill people, they’d just stop publishing anything. Instead, they’re the only agency that actually *cares* about rare side effects. You think that’s bad? Try being the guy who has to explain why a drug that helps 99% of people shouldn’t get pulled because 2 people got a weird infection. The system’s flawed? Sure. But it’s still the most rigorous in the world. Stop screaming. Start reading.
Random Guy
February 12, 2026 AT 02:17bro i just read this and my brain exploded. like… i was on that diabetes med and now i’m scared to pee. what if my junk turns into a horror movie?? 😭
Tom Forwood
February 12, 2026 AT 08:49As a guy who’s lived with type 2 for 15 years, I’ve seen this movie 3 times. Every time, the panic is worse than the actual risk. I remember when the SGLT2 alert dropped - my whole neighborhood was on Reddit freaking out. Meanwhile, I’m sitting there thinking: ‘I’ve got a 1 in 5,000 chance of getting a rare infection… and a 1 in 2 chance of having a stroke if I stop my meds.’ The FDA didn’t say ‘stop.’ They said ‘watch for pain.’ That’s it. That’s the whole thing. You don’t need a PhD to get it. You just need to not let fear do your thinking for you. And yeah - talk to your doc. They’re not just there to write prescriptions. They’re your filter.
John McDonald
February 13, 2026 AT 14:51Just want to say - this is one of the clearest breakdowns I’ve seen. The ‘signal vs. confirmed risk’ distinction is everything. I work in pharma comms and can tell you - the FDA’s internal teams are drowning in data. They’re not trying to scare you. They’re trying to catch something before it becomes a public health disaster. And honestly? They’re getting better. The 2025 updates with visual risk charts? That’s going to change everything. Imagine being able to plug in your age, condition, and meds and seeing a bar chart of risk vs benefit. No more guessing. Just facts. That’s what real transparency looks like.
Jacob den Hollander
February 15, 2026 AT 11:56I just want to say thank you for this. I’m a nurse, and I’ve had so many patients come in terrified because of these alerts. One woman stopped her antidepressant because of a vague ‘potential signal’ - and ended up in the ER with severe withdrawal. She didn’t know the risk of untreated depression was 10x higher than the ‘risk’ they were scared of. I’ve started printing out the FDA’s risk numbers for my patients. Now they can see it: ‘0.2 cases per 1,000’ - that’s like winning the lottery backwards. It helps. People need to know the numbers. Not just the scare words. The FDA’s not perfect - but they’re trying. We just need to help them be heard.
John Watts
February 16, 2026 AT 09:03This is exactly why I started teaching my patients to read FDA alerts like a detective. You don’t need to be a doctor. You need to ask: ‘Is this a signal or a verdict?’ ‘How rare?’ ‘What’s the alternative risk?’ I had a guy on blood thinners who wanted to quit because of a ‘possible bleeding risk.’ I showed him the stats: 0.1% chance of major bleed vs. 12% chance of stroke if he stopped. He stayed on it. He’s still here. That’s the power of context. The FDA’s job isn’t to give you comfort. It’s to give you truth. And truth, even when scary, is better than fear.
Randy Harkins
February 16, 2026 AT 22:45❤️ This is so important. I’ve been on an SSRI for 8 years. When the pregnancy alert dropped, I was terrified. Then I looked up the numbers - 0.7% increase? That’s less than the risk of being in a car accident on the way to the pharmacy. I talked to my OB. She said, ‘Your depression is the real threat.’ I cried. Not from fear. From relief. Thank you for saying this. We need more of this. Not fear. Facts. 🙏
Tori Thenazi
February 17, 2026 AT 06:42Wait… wait… so you’re telling me the FDA isn’t secretly controlled by Big Pharma?? 😳 I thought the ‘potential signal’ was just a cover-up for corporate greed! I mean… what if the ‘0.2 cases’ are actually 200,000 and they’re just hiding it?! They’ve been doing this since the 90s with Vioxx!! They’re lying to us!! I read on a blog that the FDA deletes reports… I think my meds are making me sleepwalk… I need to go to the moon…
Elan Ricarte
February 17, 2026 AT 12:03Let’s be real - the FDA’s like that one cousin who shows up to Thanksgiving with a PowerPoint titled ‘Why Your Turkey Is a Biohazard.’ They’re trying to be helpful. But they’re also the reason your aunt won’t eat turkey anymore. ‘Potential signal’? Bro, that’s just corporate-speak for ‘we saw something weird and we’re too scared to say ‘maybe it’s nothing.’’ Meanwhile, you’re sitting there with your hand on your pill bottle like it’s a live grenade. Chill. The risk of stopping is usually 10x worse. And yeah - your doctor’s the only one who can tell you if this is a ‘uh-oh’ or a ‘meh.’
Angie Datuin
February 19, 2026 AT 06:50Thank you for writing this. I’ve been on a drug for anxiety for 5 years. When the alert came out, I didn’t know what to do. I didn’t want to stop, but I didn’t want to risk anything either. I called my doctor. She said, ‘The risk is 1 in 5,000. Your anxiety without this? 1 in 3.’ I stayed on it. I’m okay. I just needed someone to say: ‘It’s not a death sentence.’
Camille Hall
February 21, 2026 AT 04:13One thing I wish more people understood: the FDA doesn’t issue alerts to scare you. They issue them because someone - maybe a nurse, maybe a patient - reported something unusual. That’s how we catch problems early. It’s not perfect. But it’s how we learn. And if you’re reading this and you’re scared? Talk to your doctor. Not Reddit. Not TikTok. Your doctor. They know your body. They know your history. And they’re not trying to sell you anything. They’re trying to keep you alive.