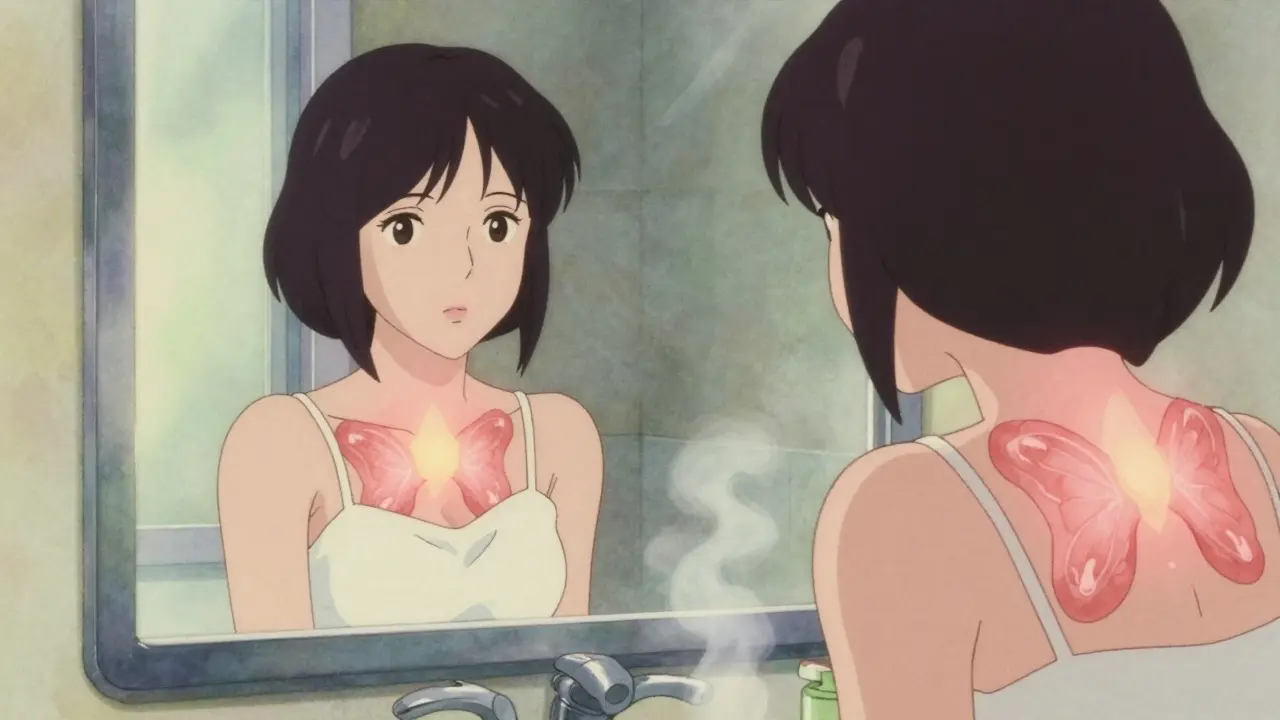
A goiter isn’t just a lump in the neck-it’s a sign your thyroid is working overtime, struggling to make enough hormones. It can swell slowly over years, or appear suddenly after pregnancy or illness. For many, it’s silent until they catch a glimpse in the mirror or feel tightness when swallowing. In places without iodized salt, it’s still common. In places like the U.S., it’s often tied to something deeper: your immune system turning on your own thyroid.
What Exactly Is a Goiter?
A goiter is simply an enlarged thyroid gland. The thyroid sits at the base of your neck, shaped like a butterfly. In a healthy person, it weighs about 15 to 20 grams-roughly the size of a small almond. When it grows beyond 25 mL in volume (about the size of a walnut), it’s considered abnormal. Some goiters stay small and cause no trouble. Others grow large enough to press on your windpipe, making breathing hard, or on your esophagus, making swallowing feel like there’s a lump stuck in your throat. Hoarseness, coughing, or a feeling of fullness in the neck are common signs.
The thyroid doesn’t swell for no reason. It’s trying to compensate. If it’s not getting enough iodine, it grows bigger to trap more of it. If your immune system is attacking it, the gland swells in response to the damage. It’s not cancer. It’s not always serious. But it’s your body’s way of saying something’s off.
Iodine Deficiency: The Global Cause
Around the world, iodine deficiency is responsible for about 90% of goiter cases. That’s not a small number-it’s the main reason millions still live with visible neck swellings. Iodine is a mineral your body can’t make. You need it to produce thyroid hormones, which control your metabolism, body temperature, and brain development. Without enough iodine, your thyroid starts overworking, growing larger to catch every bit it can.
In the early 1900s, parts of the U.S. Midwest had goiter rates over 70% in some towns. Then came iodized salt. Dr. David Marine’s 1917 study in Ohio schoolgirls proved that adding just a tiny amount of iodine to salt cut goiter rates by over 80%. By the 1920s, the U.S. made iodized salt standard. Today, in countries with strong public health programs, iodine deficiency is rare.
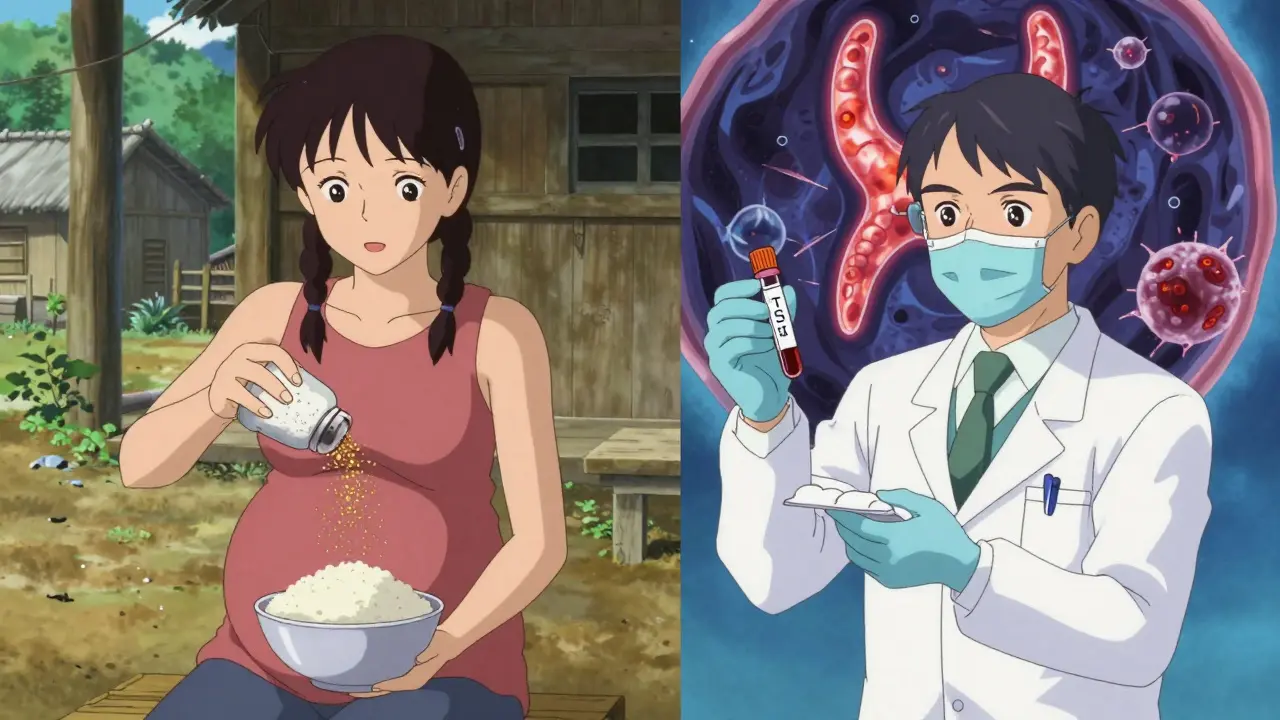
But globally, 1.9 billion people still live in areas where soil and water lack iodine. The World Health Organization says universal salt iodization has cut goiter rates by half since the 1990s. Still, many don’t have access. In these regions, children are especially at risk-not just for goiter, but for developmental delays. Pregnant women need extra iodine too. Without it, their babies can suffer irreversible brain damage.
Why Goiter Is Different in the U.S.
In the U.S., iodine deficiency is rare because of salt fortification. But goiter is still common-about 5% of the population has one. Why? Because the cause changed. Now, the biggest culprit is autoimmune disease.
Hashimoto’s thyroiditis is the most common. Your immune system mistakes your thyroid for a threat and attacks it. The gland swells, then slowly gets damaged. Over time, it can’t make enough hormones, leading to hypothyroidism. Fatigue, weight gain, cold intolerance-those symptoms often follow the swelling.
Graves’ disease is another autoimmune cause. Here, your immune system overstimulates the thyroid. The gland grows too big and pumps out too much hormone. This causes a toxic goiter-weight loss, rapid heartbeat, anxiety, and tremors. It’s rarer than Hashimoto’s, but it’s the reason some goiters come with hyperthyroidism.
Women are three times more likely than men to develop goiter. Risk rises after 40. If you have a family history of thyroid disease, your chances go up even more.
How Much Iodine Do You Really Need?
The Recommended Dietary Allowance (RDA) for iodine is 150 micrograms (mcg) per day for adults. During pregnancy, it jumps to 220 mcg. While breastfeeding, you need 290 mcg. That’s not much-but it’s essential.
One gram of iodized salt contains about 45 mcg of iodine. So if you use half a teaspoon (about 3 grams) of iodized salt daily, you’re getting roughly 135 mcg. That’s close to the daily target. But many people don’t use salt that way. They eat processed foods, which often use non-iodized salt. Or they switch to sea salt or Himalayan salt, which rarely contains added iodine.
Other sources include dairy products, eggs, seafood, and some breads. But if you’re vegan, avoid dairy, or eat little seafood, you might not get enough. That’s why prenatal vitamins in the U.S. now include iodine-because diet alone isn’t always enough.
Iodine Supplementation: Does It Work?
If your goiter is from iodine deficiency, supplementation works. Giving 150 mcg of iodine daily for 6 to 12 months typically shrinks the thyroid by 30 to 40%. In 70 to 85% of cases, the goiter disappears completely within a year or two.
But here’s the catch: if your goiter is from Hashimoto’s or Graves’ disease, iodine won’t fix it. In fact, too much iodine can make autoimmune thyroid problems worse. That’s why doctors test for thyroid antibodies before recommending supplements. If you have Hashimoto’s, extra iodine can trigger a flare-up.
Public health programs use potassium iodide in doses of 90-150 mcg for kids and 150-250 mcg for adults and pregnant women. These are safe, controlled doses. But self-supplementing with high-dose iodine pills? That’s risky. Some supplements contain 100 to 500 times the RDA. That can cause thyroid dysfunction-even in people who didn’t have a problem before.
Other Treatments: Beyond Iodine
If iodine doesn’t help, or if the goiter is large and pressing on your airway, other options exist.
For Hashimoto’s-related hypothyroidism, levothyroxine is the go-to. It replaces the missing hormone and can shrink the goiter by 10 to 20%. But because the gland becomes scarred over time, it rarely goes away completely.
For toxic goiters from Graves’ disease, antithyroid drugs like methimazole (5-30 mg daily) are used. These stop the gland from overproducing hormones. Within 12 to 18 months, the goiter shrinks by 40 to 60%. But relapse is common after stopping the drugs.
Radioactive iodine is another option. It destroys overactive thyroid tissue. It’s effective-reducing volume by 50 to 60% in 6 to 12 months. But 75 to 80% of people end up with permanent hypothyroidism. That means lifelong daily medication.
Surgery is reserved for very large goiters-over 80 to 100 mL-or when there’s compression. A total thyroidectomy removes 30 to 40 grams of tissue. It’s effective, but carries risks: voice changes in 15% of cases, low calcium levels in 8%. Patient satisfaction with surgery is only 42%, according to post-op reviews.

What About Selenium?
You might see selenium advertised as a thyroid support supplement. It’s a mineral involved in thyroid hormone metabolism. Some studies in Europe suggest it might help reduce inflammation in Hashimoto’s patients. But the Cochrane Review in 2021 found no significant benefit for goiter reduction. The odds of improvement were nearly the same as placebo. European Thyroid Association guidelines say it *might* help in specific cases, but it’s not standard care. Don’t spend money on selenium pills unless your doctor recommends it.
What’s New in Goiter Research?
Scientists are now looking at genetics. The NIH-funded TRIPOD study, launched in 2023, is tracking 5,000 people across 10 countries. Early data shows 37 genetic locations linked to thyroid size. That means some people are just more prone to goiter, even with enough iodine.
Regulations are tightening too. The FDA now requires iodine content to be labeled on all salt products. In Europe, radioactive iodine dosing is being standardized to reduce side effects.
The global market for thyroid treatments is growing. It was worth $4.7 billion in 2022 and is expected to hit $6.3 billion by 2027. Levothyroxine alone is prescribed over 120 million times a year in the U.S. That tells you how common thyroid problems are.
What Should You Do If You Suspect a Goiter?
If you notice a swelling in your neck, don’t ignore it. See a doctor. They’ll check your thyroid with a physical exam and likely order blood tests for TSH, free T4, and thyroid antibodies. An ultrasound will measure the size of the gland.
Don’t start taking iodine supplements on your own. If you’re pregnant or planning to be, talk to your doctor about prenatal vitamins with iodine. If you’re vegan or avoid dairy, ask about dietary sources or a supplement. But if you have a history of thyroid disease, iodine could do more harm than good.
Most goiters are manageable. With the right diagnosis, treatment works. Iodine deficiency is fixable. Autoimmune goiters are controllable. Even large ones can be treated safely. The key is not to guess-get tested.