Why Your Medications Are Making Your Eyes Feel Like Sandpaper
If you’ve been popping pills for high blood pressure, depression, allergies, or acne and suddenly your eyes burn, sting, or feel gritty-especially after staring at a screen-you’re not imagining it. Dry eyes from medication is a real, widespread issue that’s often overlooked. It’s not just aging or too much screen time. It’s your prescriptions. Up to 30% of all dry eye cases come from drugs you’re taking daily. For people over 65 on multiple medications, that number jumps to 40%. And many doctors don’t even ask about it.
Medications mess with your tear film in four main ways. Some block the nerves that tell your tear glands to produce tears. Others dry you out systemically, like diuretics that make you pee more. Some damage the tiny oil glands along your eyelids, which keep tears from evaporating too fast. And some eye drops themselves-yes, the ones meant to treat glaucoma-are full of preservatives that burn your eyes over time.
Which Medications Are Most Likely to Cause Dry Eyes?
You might be surprised by the list. It’s not just the obvious ones. Here are the big offenders:
- Antihistamines like Benadryl, Claritin, and Zyrtec-designed to stop runny noses, but they also shut down tear production.
- Antidepressants including Zoloft, Prozac, amitriptyline, and nortriptyline-these change brain chemicals, but they also reduce signals to your tear glands.
- Blood pressure meds like metoprolol, atenolol, hydrochlorothiazide, and Lasix-they lower blood pressure by flushing fluid out of your body, and your eyes are one of the first places it shows.
- Acne treatments like Accutane (isotretinoin)-this one is brutal. It shrinks oil glands all over your body, including those in your eyelids. Many users say their eyes never fully recover.
- Glaucoma eye drops like latanoprost and timolol-up to 47% of users get dry, burning eyes because of the preservative benzalkonium chloride (BAK). Switching to preservative-free versions cuts that number in half.
- Newer drugs like immune checkpoint inhibitors for cancer, DPP-4 inhibitors for diabetes, and EGFR inhibitors for skin conditions-are now being linked to dry eye in clinical studies.
It’s not about taking one pill. It’s about stacking them. The more meds you take, the higher your risk. And if you’re on a combination of antihistamines, antidepressants, and a diuretic? Your eyes are in the danger zone.
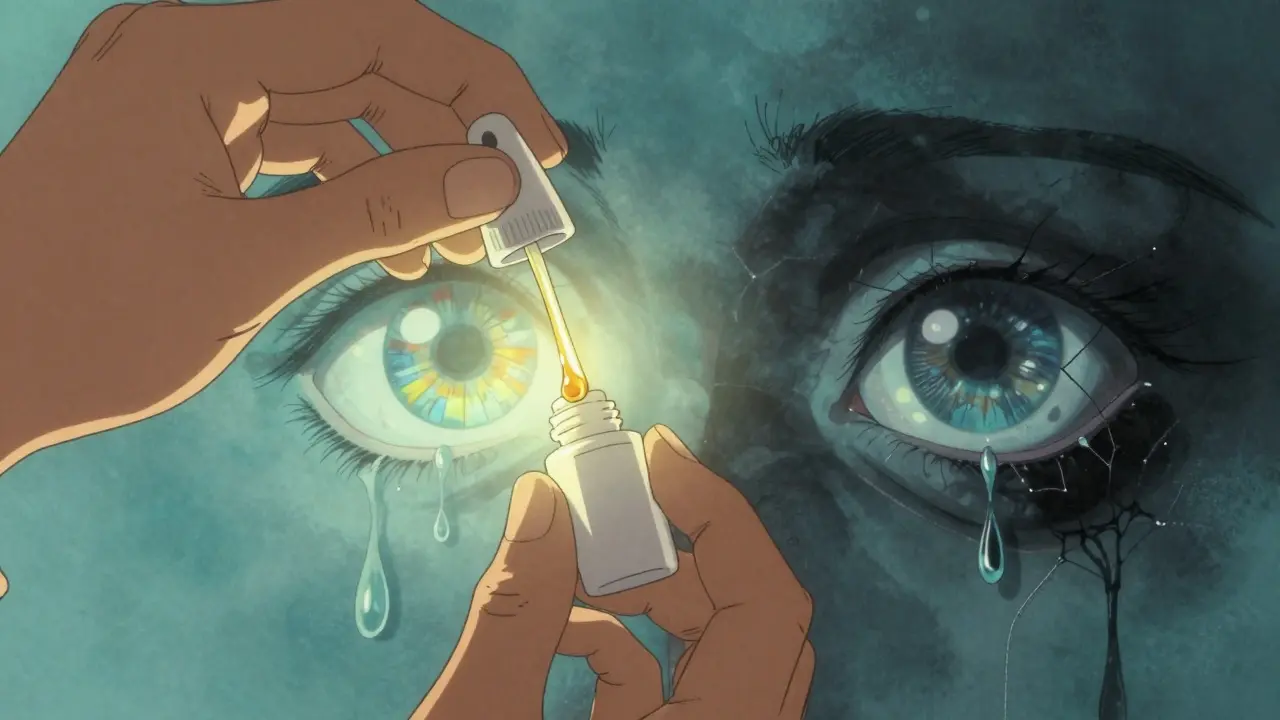
Lubrication: What Actually Works (And What Doesn’t)
Not all eye drops are created equal. Most over-the-counter drops have preservatives like benzalkonium chloride. That’s fine if you use them once or twice a day. But if you’re using them four or five times a day-which you likely need to do-those preservatives start irritating your eyes more than helping.
Preservative-free artificial tears are the gold standard. They come in single-use vials or special pump bottles that keep bacteria out without chemicals. Use them 4 to 6 times a day. Don’t wait until your eyes feel bad. Use them before you get symptoms-morning, after lunch, before dinner, and at bedtime.
If you’re using glaucoma drops, time matters. Wait at least 15 minutes between your prescription drops and your lubricating drops. Otherwise, you’re washing out the medicine before it can work. Studies show this simple timing trick improves symptoms by 78%.
For stubborn cases, doctors prescribe:
- Restasis (cyclosporine)-takes 3 to 6 months to work, but boosts natural tear production by 15-20%.
- Xiidra (lifitegrast)-reduces inflammation and dryness in about 30% of users within 2 weeks.
- Cequa-a newer version of cyclosporine with nanomicellar tech that’s 300% more effective than older formulas.
For severe cases, tiny plugs can be inserted into the tear ducts to keep your tears from draining away too fast. Temporary collagen plugs last 3-6 months and give you a test run. Permanent silicone plugs can last years. Both increase tear volume by 40-50%.
Lifestyle Fixes That Actually Make a Difference
Medication changes take time. Lubrication helps-but lifestyle tweaks give you back your daily comfort faster.
- Use a humidifier-especially in winter or in air-conditioned rooms. Keeping humidity between 40% and 60% cuts tear evaporation by 25%.
- Follow the 20-20-20 rule-every 20 minutes, look at something 20 feet away for 20 seconds. This isn’t just for screen fatigue. It forces your eyes to blink properly. People on antidepressants or antihistamines blink 40% less when staring at screens. This rule cuts digital eye strain by 35%.
- Take omega-3s-1,000 to 2,000 mg of EPA and DHA daily. Fish oil or algae-based supplements. Studies show 60% of users see better tear stability within 3 months. It’s especially helpful if you’re on diuretics or Accutane.
- Avoid direct airflow-don’t sit where your car vent, fan, or AC blows straight at your face. Air moving faster than 0.15 meters per second near your eyes doubles tear evaporation.
- Quit smoking-smoke makes dry eye symptoms 45% worse. If you stop, you’ll notice improvement in 2 to 4 weeks.
- Warm compresses and lid massage-heat your eyelids for 10-15 minutes twice a day, then gently massage along the lash line. This melts the clogged oil in your meibomian glands. Works in 65% of people on Accutane or other gland-damaging drugs.
When to Talk to Your Doctor-And What to Say
Don’t just live with it. Don’t assume it’s “just dry eyes.” Your doctor needs to know this is happening.
Bring your full medication list-not just the ones you think matter. Ask:
- “Could any of these be causing my dry eyes?”
- “Is there a similar medication without this side effect?”
- “Can we try lowering the dose?”
Studies show that adjusting the dose or switching drugs helps 55% of patients. But never stop or change a medication on your own. Stopping blood pressure or antidepressant meds suddenly can be dangerous. Work with your doctor and your eye specialist together.
Some doctors now use tools like tear osmolarity tests and meibomian gland imaging to see exactly how your eyes are affected. Ask if your eye doctor offers these tests. They’re becoming standard in major clinics.
What Doesn’t Work (And Why You’re Wasting Money)
There’s a lot of noise out there. Here’s what doesn’t help-or makes things worse:
- Preserved eye drops more than 4 times a day-the preservatives build up and damage your surface.
- Drinking more water alone-yes, hydration matters, but if your tear glands are blocked or shut down by meds, drinking a gallon of water won’t fix it.
- “Natural” remedies like aloe vera or honey in the eye-no scientific backing. Risk of infection.
- Waiting until symptoms are unbearable-dry eye gets worse over time. The longer you wait, the harder it is to reverse.
And yes, cost is a real problem. Restasis costs around $550 a month in the U.S. without insurance. Many patients struggle to get coverage. Ask your doctor about samples, patient assistance programs, or generic alternatives. Some preservative-free drops now cost under $20 for a 30-day supply.

Real People, Real Results
On Reddit’s r/dryeye community, thousands share their stories. One user on Zoloft said: “My eyes felt like sandpaper. After switching to preservative-free Systane Ultra and doing warm compresses twice a day, I could read for more than 20 minutes without burning-within two weeks.”
Another on Accutane tried everything. Nothing worked until she got iLux thermal pulsation therapy-a 15-minute in-office treatment that melts blocked oil glands. It cost $500 per session, but she got 80% relief.
These aren’t miracles. They’re targeted fixes. You don’t need to spend thousands. You just need to know what’s broken-and how to fix it.
What to Expect and How Long It Takes
Don’t give up after a few days. Dry eye from meds is a slow burn.
- 2-4 weeks: You’ll notice less burning and grittiness with consistent lubrication and lifestyle changes.
- 3-6 months: Prescription drops like Restasis or Cequa start showing real improvement in tear production.
- 6-12 months: If you’ve switched meds or stopped a damaging drug (like Accutane), your glands may begin recovering.
Adherence is everything. The Tear Film and Ocular Surface Society says 60% of success comes from sticking to the full plan-not just using drops once in a while.
Pro tip: Apply drops correctly. Tilt your head back, pull your lower lid down gently, and let the drop fall in without touching the bottle to your eye. Touching the eye contaminates the bottle and reduces effectiveness by 25%.
The Bigger Picture: Why This Matters Now
The global dry eye market is set to hit $8 billion by 2030. Why? Because more people are on more meds-and more doctors are finally paying attention.
The FDA now encourages drugmakers to make eye drops without preservatives. New formulations are coming. Preservative-free options now make up 35% of the market-up from 15% just five years ago.
But the real win? Coordination. When your primary care doctor, psychiatrist, or cardiologist talks to your eye doctor, outcomes improve. Dry eye is no longer just an “eye problem.” It’s a whole-body side effect that deserves a whole-body solution.

Jane Lucas
December 27, 2025 AT 16:12switched to preservative-free drops and now i can actually read without crying
dean du plessis
December 29, 2025 AT 01:47now i get why my contacts feel like theyre glued to my eyeballs
Gerald Tardif
December 30, 2025 AT 14:28took me three years to figure out my Accutane was nuking my tear ducts
now i do warm compresses like it's yoga and my eyes thank me
Liz Tanner
December 31, 2025 AT 02:29Liz MENDOZA
December 31, 2025 AT 06:44Robyn Hays
December 31, 2025 AT 11:49Kishor Raibole
December 31, 2025 AT 23:01Elizabeth Alvarez
January 2, 2026 AT 07:52Babe Addict
January 3, 2026 AT 19:54Paula Alencar
January 5, 2026 AT 06:46Satyakki Bhattacharjee
January 5, 2026 AT 22:38Monika Naumann
January 7, 2026 AT 01:18